Meltdown vs Shutdown Autism: 7 Critical Truths for Parents

The house finally got quiet.
After forty minutes of chaos—the screaming, the throwing, the neighbors probably wondering if they should call someone—your child collapsed into their bed. Eyes closed. Breathing steady. The storm passed.
You exhaled for the first time in an hour.
Finally. They’re calm.
Except here’s what I didn’t understand for years, what none of the parenting books prepared me for, what changed everything once I finally learned it:
Sometimes quiet isn’t calm. Sometimes it’s collapse.
Sometimes when our kids stop fighting, they haven’t found peace. They’ve just run out of gas.
And the difference between those two states—between a meltdown and a shutdown—matters more than most parents realize. Because how we respond to each one shapes whether our kids feel safe enough to keep showing us when they’re struggling, or whether they learn to suffer alone where we can’t see them.
This isn’t about labels. It’s not about making excuses or pathologizing normal kid behavior.
This is about learning to see what’s actually happening beneath the surface so we can respond in ways that help instead of accidentally making things worse.
The 7 Critical Truths About Meltdown vs Shutdown Autism
Before we dive deep, here’s what every parent needs to understand:
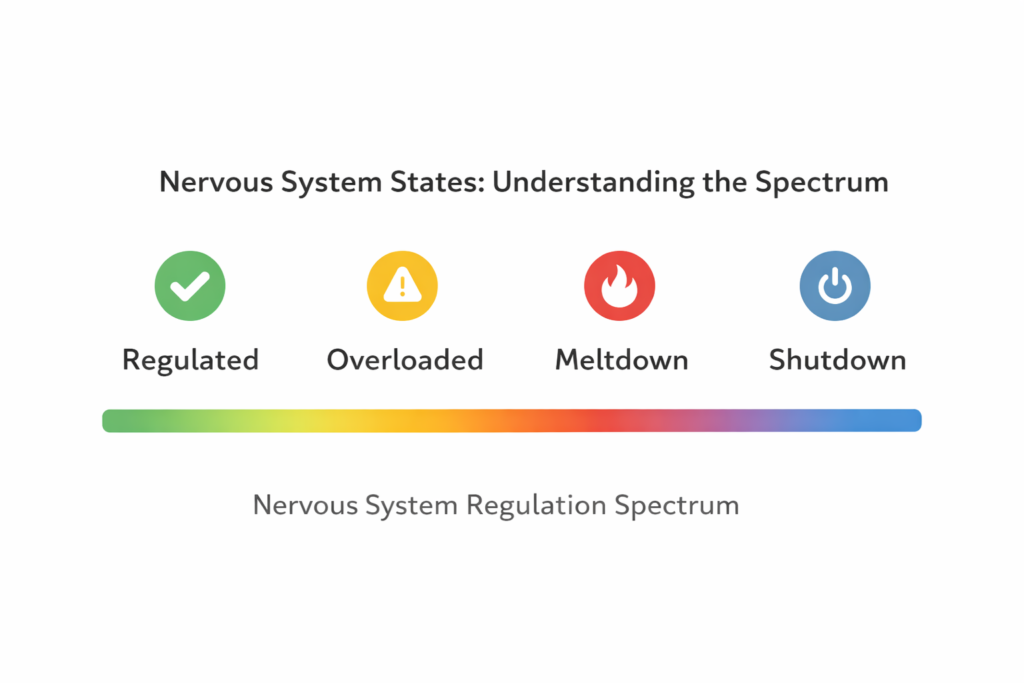
- Meltdowns and shutdowns are both nervous system responses—not behavior choices or discipline issues.
- Meltdowns are outward (visible, explosive, demanding attention), while shutdowns are inward (quiet, withdrawn, easily missed).
- Quiet doesn’t equal calm—a child in shutdown is still in crisis, just invisibly.
- Traditional discipline backfires during both because the brain’s reasoning centers are offline.
- Praising shutdowns as “good behavior” accidentally teaches kids to hide their distress.
- Both require safety and reduced input—not lessons, consequences, or forced processing.
- Being seen correctly builds trust—which is the foundation for long-term emotional regulation.
Now let’s break down exactly what that means and how to respond.
Quick Recognition Guide:
🔥 Meltdown (Fight/Flight): Loud, movement, yelling/crying, throwing things, pacing, hitting, “can’t stop”
🧊 Shutdown (Freeze): Quiet, still, blank/flat affect, speech drops or disappears, retreats inward, “can’t start”
Meltdown vs Shutdown: At-a-Glance Comparison

| What You Need to Know | Meltdown (Fight/Flight) | Shutdown (Freeze) |
|---|---|---|
| What You See | Explosive, loud, physical movement, crying/yelling, throwing/hitting | Quiet, withdrawn, blank expression, minimal movement, non-responsive |
| What’s Happening Inside | Nervous system in overdrive, sensory overload spilling out, can’t contain the overwhelm | Nervous system conserving energy, retreating inward to survive, emotional numbing |
| What NOT to Do | Talk too much, demand explanations, give consequences immediately, restrain unless safety requires it | Praise the quiet, push them to reengage, treat it as resolved, ask them to explain themselves |
| What Helps Most | Reduce sensory input, simplify language to 1-2 words, ensure physical safety, stay regulated yourself | Offer calm presence without demands, respect their recovery pace, maintain routines quietly, don’t force processing |
| Best Anchor Phrase | “I’m here. You’re safe. We’ll talk later.” | “I’m going to sit here. You don’t have to talk. I’m just here.” |
| How It Usually Resolves | When nervous system stabilizes (often 20-45 minutes), physical exhaustion sets in, sensory load reduces enough | Slowly, over hours sometimes, as internal energy rebuilds, when they feel safe enough to reengage |
| Common Misreading | Seen as tantrum, manipulation, or defiance | Seen as calm, compliance, or “finally behaving” |
Why Understanding Meltdown vs Shutdown Autism Changes Everything
Here’s what nobody told me when we first started navigating autism with our kids: the nervous system doesn’t respond to logic in that moment.
When your child melts down, when they shut down, when they lose access to language or eye contact or the ability to hear your voice—that’s not a choice. That’s not manipulation. That’s not them “being difficult” or “needing firmer boundaries.”
That’s their autonomic nervous system hitting overload and doing exactly what it’s designed to do: protect them from what feels like a threat.
The problem? As adults, we’ve been conditioned our whole lives to associate certain behaviors with certain intentions:
- Yelling = disrespect
- Silence = compliance
- Sitting still = listening
- Looking away = ignoring
But in autistic kids (and honestly, in a lot of neurotypical kids too), those equations don’t hold. A child who goes silent after a meltdown might not be “finally listening.” They might be so overwhelmed their brain literally cannot process language anymore.
A child who stops arguing might not have accepted your point. They might have shut down so completely they can’t access the part of their brain that forms words.
And if we keep responding to shutdowns the way we respond to meltdowns—or worse, if we treat shutdowns as “finally behaving”—we teach our kids something devastating:
The only safe way to be overwhelmed is to disappear.
I’ve written before about disciplining autistic children and how traditional consequences often backfire. But this goes deeper than discipline. This is about interpretation. About learning to read the signals our kids are sending when they can’t use words to tell us what’s happening.
Because how we interpret behavior shapes how safe our kids feel expressing distress in the first place.
What a Meltdown Actually Is (And What It Isn’t)
Let me paint you a picture from our house.
Melody, age 15, standing in the kitchen. I asked her to unload the dishwasher—something she’s done a thousand times. Simple request. No big deal.
Except it was a big deal.
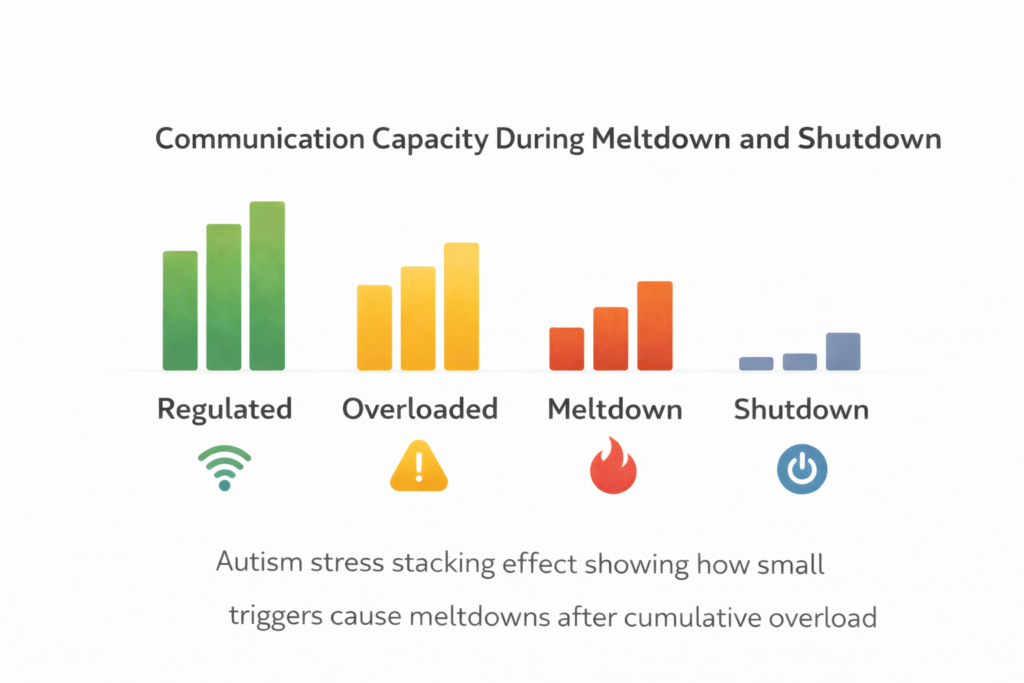
Because what I didn’t see: she’d already navigated a loud cafeteria at lunch, fluorescent lights buzzing all day, three unexpected schedule changes, a substitute teacher who didn’t understand she needed the classroom door closed, and a friend group drama that required her to mask her confusion for six straight hours.

So when I asked her to unload the dishwasher, what I was really asking was: Can you do one more thing when your nervous system is already at 147% capacity?
The answer was no.
But her brain couldn’t form that sentence. Instead, it went straight to fight-or-flight. Plates got slammed. Silverware clattered across the counter. She yelled something about everyone always asking her to do everything (which objectively wasn’t true, but felt true to her overloaded system).
That’s a meltdown.
Here’s What Meltdowns Actually Are:
Meltdowns are involuntary nervous system overload responses. They happen when the brain’s capacity to process input—sensory, emotional, social, cognitive—gets completely maxed out.
Think of it like a circuit breaker. When too much electricity flows through the system, the breaker flips. Not because it’s broken. Because it’s working exactly as designed to prevent bigger damage.
During a meltdown:
- ⚡ The sympathetic nervous system activates (fight-or-flight)
- 🧠 Access to rational thinking drops dramatically
- 💬 Language processing gets severely impaired
- 🎯 Executive function becomes extremely limited
- 🔊 Sensory sensitivity spikes even higher
Meltdowns are outward. Visible. Disruptive. They demand attention because the nervous system is screaming “SOMETHING IS WRONG AND I CAN’T COPE.”
Here’s What Meltdowns Are NOT:
Let me clear up some common misunderstandings that make everything harder:
❌ Not tantrums. Tantrums have a goal (get the toy, avoid bedtime, gain control). Meltdowns have no goal. They’re pure overwhelm with no off switch.
❌ Not manipulation. Nobody melts down on purpose. Would you choose to lose control of your body and emotions in front of people? Of course not. Neither do our kids.
❌ Not a discipline issue. You can’t punish someone out of a nervous system response any more than you can punish someone out of a panic attack.
❌ Not something kids can “just stop” if they tried harder. During a meltdown, the parts of the brain that control impulse, reasoning, and self-regulation are temporarily offline. Demanding they “calm down” is like telling someone having a seizure to “just relax.”
Here’s the meaning behind this: Meltdowns are the body’s emergency release valve. They’re what happens when there’s no other way to discharge the overload.
And the worst part? Every meltdown teaches our kids something about themselves. Either they learn “I lost control and the adults helped me feel safe again,” or they learn “I lost control and proved I’m bad/broken/too much.”
Which lesson they take away depends entirely on how we respond. (More on that in a minute.)
Parent Note 📝
If you’re asking “Is this a tantrum or meltdown?” the fastest clue is this: tantrums change when the audience changes. Meltdowns usually don’t.
What a Shutdown Is (And Why It Gets Missed So Often)
Now let me tell you about the day I almost completely misread my own kid.
Gabrielle, age 13, came home from youth group. I asked how it went.
“Fine.”
How was the game night?
“Good.”
Did you have fun with your friends?
“Yeah.”
She went to her room. Closed the door quietly. Didn’t come out for dinner. When I checked on her, she was lying on her bed, staring at the ceiling, completely still.
No tears. No yelling. No obvious distress.
From the outside, she looked… fine. Quiet. Maybe tired.
From the inside? She was drowning.
That’s a shutdown.
Here’s What Shutdowns Actually Are:
Shutdowns are inward responses to overwhelm. Instead of the nervous system going into fight-or-flight (outward release), it goes into freeze (inward collapse).
Autistic adults often describe shutdown as entering a “power-save mode” after overload—the body conserving every bit of energy just to exist.
The brain says: “I can’t handle any more input. I’m shutting down non-essential systems to survive this moment.”
During a shutdown:
- 🔋 Energy drops dramatically
- 💬 Speech becomes difficult or impossible
- 👁️ Eye contact feels unbearable
- 🎭 Emotional expression flattens
- 🧊 The child appears “checked out” or “zoned out”
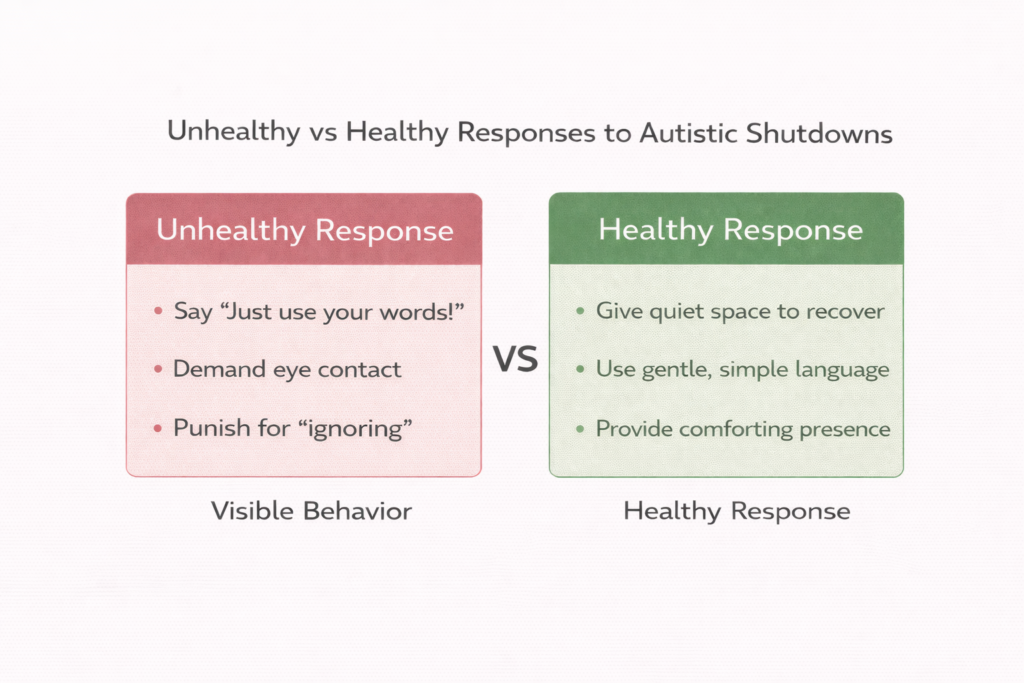
But here’s the critical part most parents miss: shutdowns look calm from the outside.
No noise. No destruction. No drama. Just a kid who seems… compliant. Mature. “Finally settling down.”
Except internally, their nervous system is still in full crisis mode. They’re not calm. They’re conserving every ounce of energy just to exist without falling apart completely.
(Yes, I realize this sounds dramatic, but stay with me here—this is exactly how autistic adults describe it, and once you understand it, so much behavior suddenly makes sense.)
Why Shutdowns Get Misread as “Good Behavior”
This is where things get dangerous.
Because we live in a world that rewards:
- ✅ Quiet over loud
- ✅ Still over moving
- ✅ Compliant over resistant
- ✅ “Under control” over “making a scene”
So when a kid who was just screaming and throwing things an hour ago suddenly goes silent and docile, what do most of us think?
“Finally. They calmed down. Crisis over.”
But that’s not what happened.
What happened is their nervous system ran out of fight. They didn’t regulate. They didn’t process their emotions and arrive at peace. They collapsed under the weight of overwhelm and retreated so far inward we can’t reach them anymore.
The Counseling and Wellness Center of Pittsburgh explains that when the body’s stress response system gets overloaded, it can trigger a freeze state where the person becomes immobilized—not by choice, but by neurological design meant to protect them from further harm.
And here’s the gut-punch: We often reward this.
“See? I knew you could calm down if you tried.”
“This is much better. Why can’t you be like this all the time?”
Every time we praise a shutdown as success, we accidentally teach our kids: The way to make adults happy when I’m overwhelmed is to disappear.
Quick Takeaway 💡
If your child goes quiet after chaos, don’t assume it’s peace. Assume they’re recovering.
The Difference Between Meltdown and Shutdown: What It Feels Like Inside
Let me give you the side-by-side because this is where understanding shifts from intellectual to visceral.
What a Meltdown Feels Like Inside the Body
Imagine:
Your skin feels like it’s on fire. Every sound is a drill going through your skull. The lights are stabbing your eyes. Someone’s talking to you but their words are just noise—your brain can’t turn sound into meaning anymore.
Your heart is racing. Your muscles are clenched so tight they hurt. There’s this buzzing, vibrating feeling under your skin like you’re going to crawl out of your own body.
You know you’re yelling. You know you’re crying. You know you’re saying things you’ll regret later. But you can’t stop. The rational part of your brain that usually controls impulses? Offline. Completely unreachable.
You’re not choosing this. You’re trapped inside it, watching yourself lose control and unable to access the brakes.
That’s what autism meltdowns feel like.
And when someone tells you to “just calm down” or “use your words” or “take a deep breath,” it’s not that you won’t. You can’t. The parts of your brain that do those things aren’t online right now.
Dr. Ross Greene, who wrote The Explosive Child, puts it this way: Kids do well if they can. If they’re not doing well, it’s not because they’re choosing not to. It’s because they’ve hit a capacity limit they don’t have the skills to manage yet.
What a Shutdown Feels Like Inside the Body
Now imagine this instead:
Everything goes… quiet. Not peaceful quiet. Empty quiet.
Your body feels heavy. Like someone turned up gravity. Moving takes effort you don’t have. Talking feels impossible—not because you’re being stubborn, but because the pathway between thought and speech just… isn’t there right now.
People are asking you questions. You hear them. But answering requires energy you used up three hours ago. So you don’t. You can’t.
Your face feels frozen. You know you should smile, nod, show something, but your facial muscles won’t cooperate. Everything feels far away, like you’re watching life through frosted glass.
You’re not calm. You’re numb. Emotionally and physically depleted.
And the worst part? Everyone thinks you’re fine now. They’re relieved. They’ve moved on.
But you’re still drowning. Just silently. Where no one can see.
That’s what shutdown feels like.
Reframing Autism describes this as protective withdrawal—the nervous system’s last-resort strategy when fight and flight both failed. It’s not giving up. It’s survival mode.
How Adult Responses Can Help or Harm (Without Meaning To)
Here’s the hard truth I had to learn: Good intentions don’t always lead to helpful responses.
When Brayden (age 6, our youngest) has an autism meltdown, my first instinct is to fix it. Explain why he’s upset. Teach him a better way to handle it. Help him understand.
All reasonable goals. All completely counterproductive in the moment.
Because during a meltdown, the parts of his brain that process explanations aren’t functioning. Trying to teach him while he’s in fight-or-flight is like trying to have a rational conversation with someone who’s actively drowning.
They don’t need a swimming lesson right now. They need a life preserver.
Here are the well-meaning responses that often make things worse:
Common Reflexes That Backfire During Meltdowns:
❌ Talking too much.
“Okay, I know you’re upset, but we talked about this. Remember what we said about using gentle hands? I need you to…”
→ More words = more input = more overload.
❌ Forcing processing.
“Why did you throw that? What were you feeling? Can you tell me what happened?”
→ Language access is already compromised. Demanding it makes things worse.
❌ Immediate consequences.
“That’s it. You just lost screen time for the rest of the week.”
→ Punishment during a nervous system crisis teaches fear, not regulation.
❌ Physical restraint (unless absolutely necessary for safety).
→ Can escalate the fight-or-flight response and cause trauma.
The same pattern shows up during shutdowns, but the mistakes look different:
Common Reflexes That Backfire During Shutdowns:
❌ Praising the silence.
“See? I knew you could calm down. This is so much better.”
→ Reinforces hiding distress instead of processing it.
❌ Pushing them to reengage too quickly.
“Okay, you’ve had enough time alone. Come talk to me now.”
→ Shutdown recovery isn’t linear. Forcing it extends it.
❌ Treating it like the problem is solved.
“Well, you seem fine now. Let’s just move on.”
→ Misses the fact that they’re still in crisis, just invisibly.
❌ Asking them to explain what happened.
“Can you help me understand why you got so upset?”
→ They often don’t know. And asking forces them to relive it before they’ve recovered.
Here’s what I’ve learned through a lot of trial and error (and some really helpful guidance from our therapist):
Support isn’t about fixing the moment. It’s about matching the child’s capacity.
And capacity during emotional regulation crises is low. Way lower than we think.
What Actually Helps During a Meltdown
Alright, enough theory. Let’s get practical.
When your child is in full meltdown mode, here’s what actually helps (and what I wish someone had told me years ago):
Anchor Phrase (steal this) 🧠
“I’m here. You’re safe. We’ll talk later.”
✅ Reduce Sensory Input Immediately
- Dim the lights (or turn them off completely)
- Lower your voice (or stop talking entirely)
- Turn off music, TV, any background noise
- Clear the space of people if possible
- Remove tight clothing, tags, anything uncomfortable
The goal: Lower the total amount of input their nervous system has to process.
✅ Simplify Language to Near Zero
Instead of: “I can see you’re really upset right now, and I know this is hard, but I need you to try to take some deep breaths and…”
Try: “I’m here.” (Then silence.)
Or just your physical presence with no words at all.
If you need to give direction: “Safe hands.” Not “Stop hitting your sister, that’s not okay, we don’t…”—just two words. Safe hands.
✅ Prioritize Safety, Not Compliance
If they’re throwing things, move the breakable stuff, don’t demand they stop.
If they’re hitting, create distance, don’t lecture about gentle touches.
Your job isn’t to teach the lesson right now. Your job is to keep everyone safe while their nervous system reboots.
✅ Use Physical Grounding (If They Want It)
Some kids need deep pressure—tight hugs, weighted blankets, being squeezed.
Some kids need space—don’t touch me, don’t come near me, leave me alone.
Learn which yours needs. Don’t assume. (And know it might change depending on the day.)
✅ Stay Regulated Yourself
This is the hardest one.
Because when your kid is screaming and throwing and completely out of control, your own nervous system wants to escalate too. Fight or flight kicks in for you.
But here’s the thing: you can’t co-regulate with someone while you’re also dysregulated.
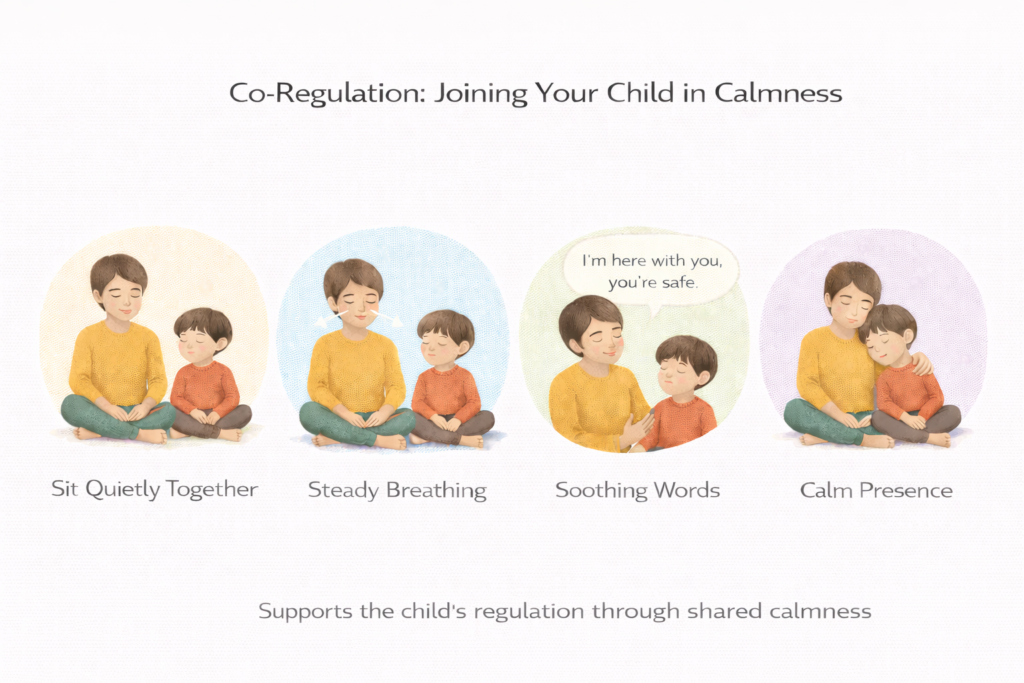
So breathe. Unclench your jaw. Drop your shoulders. Slow your own heart rate.
Your calm becomes their anchor. Your panic becomes their feedback loop.
I’ve written about creating calm spaces for autistic kids, but even the best calm space in the world won’t help if the adult in the room is radiating tension.
✅ Don’t Try to Teach or Process in the Moment
Meltdowns resolve when the nervous system stabilizes, not when the lesson is taught.
Save the conversation for later. Sometimes hours later. Sometimes the next day.
Right now? Just survive it together.
What Actually Helps During a Shutdown
Shutdowns need a completely different approach. Because the problem isn’t too much output—it’s too much input drain with nothing left to give.
Do this first ✅
Offer presence without questions. Shutdowns come back online with safety, not conversation.
✅ Offer Gentle, Predictable Presence
Sit nearby. Don’t demand interaction. Just exist in the same space.
Let them know you’re there without requiring them to respond.
“I’m going to sit here and read. You don’t have to talk. I’m just here if you need me.”
✅ Respect Their Recovery Pace
Do not push them to reengage before they’re ready.
If they need an hour alone, give them an hour.
If they need to skip dinner, let them skip dinner.
If they don’t want to talk about it, don’t make them.
Shutdown recovery is about reconnection without extraction. They’ll come back when their system has enough capacity. Forcing it just extends the shutdown.
✅ Use Minimal Language
Same as meltdowns: fewer words, softer tone, no questions that require processing.
Instead of: “Are you okay? Do you want to talk about what happened? Can I get you anything? Are you hungry? Do you need…”
Try: “Water’s on your nightstand.” (Then leave.)
✅ Maintain Routines Quietly
Routines provide safety when everything else feels chaotic.
So if bedtime is 8:30, keep bedtime at 8:30. Just adapt how you do it.
Maybe tonight they brush their teeth in silence instead of chatting about their day. That’s fine. The routine stays. The pressure goes.
✅ Don’t Interpret Shutdown as Resolution
This is critical: A child who stops reacting hasn’t necessarily finished processing.
They might just be too exhausted to show distress anymore.
So don’t treat the shutdown as “problem solved.” Treat it as “stage two of crisis management.”
The real work—helping them build skills to handle overload differently—happens after the nervous system stabilizes, not during.
⚠️ When to Get Extra Support
If meltdowns include frequent self-injury, dangerous aggression toward others, or shutdowns last multiple hours with inability to eat, drink, or communicate basic needs, talk to your pediatrician or therapist about creating a specific safety plan for your family.
Teaching Kids to Recognize Their Own Signals Over Time
Here’s where long-term change actually happens.
You can’t prevent every meltdown. You can’t avoid every shutdown. Life is unpredictable, and sensory overload doesn’t always announce itself in advance.
But what you can do is help your kids start recognizing their own patterns so they have a chance to ask for help before they hit total collapse.
This doesn’t happen overnight. It takes years. And even then, it’s not foolproof.
But it starts with naming sensations without judgment.
How We’ve Done This in Our House:
After things calm down (sometimes that same evening, sometimes the next day), I’ll check in with Melody or Gabrielle:
“Hey, I noticed you seemed really overwhelmed earlier. Do you remember what that felt like in your body?”
Sometimes they say no. Sometimes they shrug. And that’s okay—we stop there.
But sometimes they say things like:
- “My chest felt tight.”
- “Everything was too loud.”
- “I felt like I wanted to run away but I couldn’t.”
And then I reflect it back: “Yeah. That’s what overload feels like. Your body was telling you it needed a break.”
No shame. No lecture. Just: This is information. Your body sends signals. We’re learning to read them.
Over time, they start noticing earlier. “Dad, I feel really buzzy right now.” And we can adjust before it becomes a meltdown.
What This Looks Like in Practice:
🧠 Emotional literacy builds gradually. We’re not expecting a 10-year-old to have perfect self-awareness. We’re just planting seeds.
🧠 Kids need modeling, not correction. So I name my sensations too. “I’m feeling really overwhelmed right now. I’m going to step outside for a few minutes.” They learn regulation by watching us regulate.
🧠 Naming sensations builds long-term emotional regulation skills. APA guidance emphasizes treatment approaches that help kids build skills and better tolerate sensory input over time—and naming what they’re feeling is a powerful part of that process.
Here’s the meaning underneath all of this:
We aren’t trying to prevent distress. We’re teaching kids they don’t have to disappear inside it.
Because the goal isn’t to raise kids who never melt down or shut down. The goal is to raise kids who know they can fall apart and still be safe. Who know they can ask for help before it gets that bad.
Who know that losing control doesn’t mean losing connection.
Why Calm Spaces Help Differently for Meltdowns vs Shutdowns
I’ve written a lot about creating calm spaces—sensory-safe zones where kids can decompress—and they absolutely help in managing both autism meltdowns and shutdowns.
But they help differently depending on whether your child is melting down or shutting down.

During Meltdowns:
A calm space functions as a sensory reduction zone. Fewer inputs = faster nervous system recovery.
Think of it like a circuit breaker room. When the system overloads, you need a space designed to handle the surge safely until things reset.
Dim lighting, soft textures, noise-canceling headphones, weighted blankets—all of these reduce the sensory load so the brain can come back online.
During Shutdowns:
A calm space functions as a safe hideout. It’s not about reducing sensory input (they’ve already gone numb). It’s about providing a place where they don’t have to perform, mask, or engage.
A place where they can just… exist. Without demands. Without expectations. Without anyone asking them to explain themselves.
The Key Difference:
Calm spaces don’t prevent distress. They support recovery.
They don’t stop meltdowns from happening. But they help meltdowns end without shame.
They don’t cure shutdowns. But they make shutdowns feel less like abandonment and more like rest.
Here’s what I tell parents who ask if they should create a calm space: Yes. But understand it’s a tool, not a solution.
The solution is helping kids build capacity over time. The calm space just makes the hard moments survivable while they’re learning.
The Long-Term Impact of Being Seen Correctly
Let’s zoom out for a second.
Because this whole conversation—meltdown vs shutdown autism, nervous system responses, how we interpret behavior—it all comes down to one thing:
Do our kids feel seen?
Not managed. Not fixed. Not tolerated.
Seen.
When we learn to tell the difference between meltdown and shutdown, we’re not just responding better in the moment. We’re sending our kids a message that echoes through their entire development:
Your distress makes sense.
You’re not broken.
I’m learning your language.
And that message? That changes everything.
Here’s What Research Shows:
Kids who grow up feeling understood by their caregivers develop:
- Stronger emotional regulation skills (because they learn regulation with someone, not alone)
- Better communication (because they don’t have to hide or perform to be accepted)
- More resilience (because they know falling apart doesn’t mean losing connection)
- Lower rates of anxiety and depression (because they’re not carrying the weight of being misunderstood)
But kids who grow up feeling misread—who melt down and get punished, who shut down and get praised, who learn that the only safe way to be overwhelmed is to hide it—they internalize something much darker:
My emotions are wrong.
I’m too much.
I have to manage this alone.
And that becomes the foundation for a lifetime of masking, people-pleasing, and eventual burnout.
What This Looks Like in Real Life:
I think about Natalie (20, our oldest). When she was younger, I didn’t understand shutdowns yet. So when she’d go quiet after a rough day, I’d assume she was fine.
“Glad you worked through that. See? You can handle hard things.”
I meant it as encouragement. But what she heard was: Don’t let them see you struggling.
It took years to undo that. Years of her learning that shutting down wasn’t the same as coping, and that I could handle her distress without needing her to make it easier for me.
Now? When she’s overwhelmed, she tells me. “Dad, I need to shut down for a bit.” And I say, “Okay. I’ll check on you in an hour.”
No shame. No performance. Just reality.
That’s what being seen correctly creates. Trust.
And trust builds communication.
And communication builds resilience.
What This Means for Your Family Right Now
If you’re reading this and thinking, Oh no. I’ve been getting this wrong—
Stop.
You were missing information. There’s a massive difference between not knowing and not caring.
I got it wrong for years. My kids are okay. Yours will be too.
Because the beautiful thing about nervous systems is they’re adaptable. And the beautiful thing about relationships is they can heal.
Here’s what you do next:
Start Small:
1️⃣ Just notice the difference. Meltdown = outward explosion. Shutdown = inward collapse. You don’t have to respond perfectly. Just start seeing them as distinct.
2️⃣ Reduce input during both. Fewer words. Softer tone. More space. This helps in almost every scenario.
3️⃣ Stop praising quiet as success. If your child shuts down, don’t celebrate it. Just stay present and let them recover at their own pace.
4️⃣ Have the conversation later. Not during. Not immediately after. But when everyone’s calm, talk about what happened. Name it. Normalize it.
5️⃣ Be patient with yourself. You’re learning a new language. You’ll misread signals sometimes. That’s okay. Repair and keep going.
Frequently Asked Questions About Meltdown vs Shutdown Autism
How long does an autistic shutdown last?
Shutdowns can last anywhere from 30 minutes to several hours, and sometimes even into the next day. Unlike meltdowns which tend to have a clearer resolution point, shutdowns often fade gradually as the nervous system rebuilds capacity. Recovery time depends on how depleted the child was before shutdown, what triggered it, and whether they feel safe enough to reengage. Some kids bounce back after a nap; others need 24 hours of reduced demands.
Can a shutdown happen after a meltdown?
Absolutely. In fact, this is common. A child might melt down (fight-or-flight), exhaust themselves completely, and then shift into shutdown (freeze) as their system runs out of energy.
You might see: explosive behavior → collapse into quiet → hours of withdrawn, low-energy recovery.
Is a shutdown the same as ignoring you or giving the silent treatment?
No. Ignoring someone is a choice made with language and reasoning still online. Shutdown is an involuntary nervous system response where access to speech, processing, and emotional expression becomes severely limited or temporarily unavailable. A child ignoring you can usually respond if sufficiently motivated. A child in shutdown often can’t respond even when they want to—the neurological pathway isn’t functioning normally.
What’s the fastest way to help during an autism meltdown?
Reduce sensory input immediately (dim lights, lower noise, clear the space), simplify your language to 1-3 words maximum, ensure everyone’s physical safety, and stay as calm as you can. Don’t try to teach, reason, or process emotions during the meltdown. Your job is to help their nervous system stabilize, not to solve the problem that triggered it. Think: “Safe. Quiet. Present.” That’s it.
How can you tell the difference between a meltdown and a tantrum?
Tantrums have a goal and change based on audience—if you walk away, the tantrum often stops or shifts. Meltdowns don’t have a goal; they’re pure overwhelm. A child mid-meltdown usually can’t stop even if you give them what they want. Tantrums end when the child gets their way or realizes it won’t work. Meltdowns end when the nervous system regulates, regardless of getting anything. Also: tantrums don’t usually include the same level of physical exhaustion, shame, or complete loss of language that meltdowns do.
Do all autistic kids have meltdowns and shutdowns?
Not all, but many do—especially when facing sensory overload, unexpected changes, or prolonged masking. Some autistic kids primarily melt down, some primarily shut down, and some alternate between both depending on the situation and their remaining capacity. The frequency and intensity vary widely. What’s universal is that both are nervous system responses, not behavior choices, and both deserve understanding rather than punishment.
Final Thoughts: You’re Not Alone in This
Here’s the truth nobody talks about enough:
Parenting autistic kids (or any neurodivergent kids, honestly) is hard. Not in the “toddler tantrums are exhausting” way. In the “I’m learning to see the world through a completely different lens while also keeping everyone safe and fed and somewhat functional” way.
You’re going to misread signals. You’re going to respond wrong sometimes. You’re going to have days where you think, I have no idea what I’m doing.
Me too. Still. After twenty years of marriage, six kids, and more therapy appointments than I can count.
But here’s what I know for sure:
When we learn the difference between meltdown and shutdown in autistic children, we don’t just respond better.
We teach our kids they don’t have to choose between exploding or disappearing to be supported.
We teach them their distress is valid.
We teach them they can fall apart and still be loved.
And honestly? That might be the most important thing we ever teach them.
If this perspective resonated with you, we explore related topics—faith, resilience, family life, and raising kids in a complex world—across our family of blogs:
More from Our Family of Blogs:
Lifetime Family Journey – Stories, guides, and lessons from life in a big family.
Mountains Will Move – Faith, resilience, and encouragement for life’s hardest battles.
Everyday Exposed – Real talk on culture, media, and the world we’re raising our kids in.