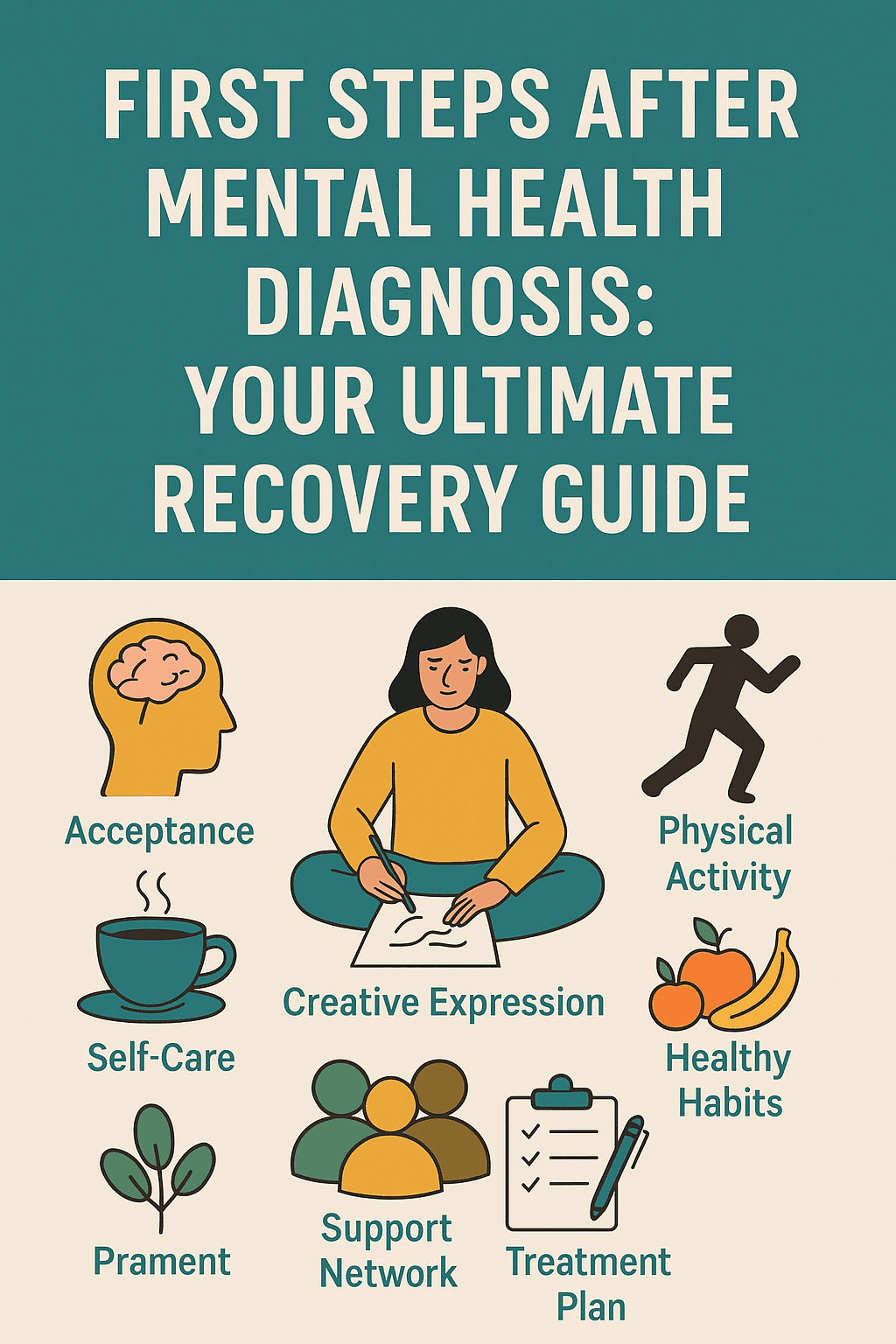
First Steps After Mental Health Diagnosis: Your Ultimate Recovery Guide
I remember staring at the prescription pad in my doctor’s hand, watching her pen move across the paper with clinical precision. The words she’d just spoken hung in the air like smoke — anxiety disorder, depression, PTSD.
After twenty-plus years of military service and raising six kids, I thought I had life figured out. Turns out, getting a mental health diagnosis doesn’t care about your background, your achievements, or how well you think you’ve been holding it together.
The silence in that office felt deafening. Not because I was ashamed, but because I honestly had no clue what came next.
If you’re reading this in the hours or days after receiving your own mental health diagnosis, I want you to know something: what you’re feeling right now — the confusion, the fear, maybe even relief — it’s all completely normal. More importantly, taking the first steps after mental health diagnosis doesn’t have to feel like walking through quicksand.
These first steps after mental health diagnosis are crucial for setting up your recovery foundation.
The Emotional Earthquake: Understanding Your Initial Reactions
✅ Your Brain Is Processing Something Big
Getting diagnosed with a mental health condition isn’t like being told you have a broken arm. There’s no visible cast for others to see, no clear timeline for healing, and definitely no instruction manual that falls out of the doctor’s folder.
The first 24 hours can feel like an emotional hurricane. One minute you might feel relieved that your struggles finally have a name. The next, you could be spiraling into worry about what this means for your future, your relationships, or your sense of identity.
I spent my first night after diagnosis ping-ponging between researching everything I could find online and avoiding the topic entirely. Both reactions are completely valid ways of coping with a new diagnosis.
💡 What Actually Happens in Your Mind
Your brain is essentially recalibrating. For months or years, you’ve been experiencing symptoms without fully understanding their origin. Now that information is reorganizing itself around this new framework, and understanding the first steps after mental health diagnosis becomes critical.
Some people describe it as puzzle pieces finally clicking into place. Others feel like their entire self-concept just got shuffled like a deck of cards.
🚨 First 48 Hours: Your Safety and Stability Checklist
Immediate Priority #1: Safety Assessment
Before anything else, you need to ensure you’re in a safe mental space. This isn’t about being dramatic — it’s about being smart. Mental health diagnoses can sometimes come with increased emotional intensity as your brain processes this new information.
Ask yourself honestly: Do you feel safe being alone right now? Are you having thoughts of harming yourself or others? If the answer to that second question is yes, please call 988 (Suicide & Crisis Lifeline) immediately or go to your nearest emergency room. This safety check represents one of the most important first steps after mental health diagnosis.
👉 Create Your 48-Hour Support Network
Identify 2-3 people who can check on you over the next two days. This doesn’t mean you have to share your diagnosis if you’re not ready. Simply ask them to call or text, maybe grab coffee, or just hang out.
I asked my wife to keep an extra eye on me during those first few days, not because I was in crisis, but because I knew my emotional baseline was shifting and I wanted someone to notice if I wasn’t acting like myself.
Essential First Steps Action Items:
These first steps after mental health diagnosis form your immediate action plan:
- Remove or secure anything you might use impulsively if emotions spike
- Stock up on comfort foods and basic necessities so you don’t have to leave the house if you don’t want to
- Set up your next appointment with your healthcare provider before leaving their office
- Write down the exact name of your diagnosis and any medications prescribed
Following these first steps after mental health diagnosis creates a foundation for everything that comes next.
Understanding Your Diagnosis Without Becoming Your Diagnosis
🧠 The Label vs. The Person
Here’s something nobody tells you about the first steps after mental health diagnosis: there’s a difference between having depression and being depressed, between experiencing anxiety and being an anxious person.
Your diagnosis is a tool for understanding and treating what you’re going through. It’s not your identity, your future, or your limitation. Learning this distinction is among the most valuable first steps after mental health diagnosis you can take.
I learned this lesson the hard way when I started introducing myself in my head as “the guy with PTSD” instead of just being me — a father, veteran, husband, and writer who happens to have PTSD. The diagnosis explains some of my experiences; it doesn’t define who I am.
Research Smart, Not Obsessively
When you’re ready to learn more about your condition, stick to reputable sources. The Mayo Clinic, National Institute of Mental Health, and American Psychological Association provide evidence-based information without the doom-and-gloom horror stories you’ll find elsewhere.
Set boundaries with your research. Give yourself 30 minutes to read, then close the computer. Information can be empowering, but information overload during those first days can amp up anxiety and make everything feel more overwhelming than it actually is. Pacing your research represents wise first steps after mental health diagnosis.
💡 Focus on What You Can Control
Your diagnosis came with treatment recommendations. These might include therapy, medication, lifestyle changes, or a combination of approaches. This is what you can control — your response to the diagnosis and your commitment to treatment.
What happened in your past that contributed to this condition? That’s largely out of your control. How your family or friends will react? Also not entirely up to you. But how you move forward with managing your mental health recovery tips? That’s 100% in your hands and represents the most empowering first steps after mental health diagnosis.
How to Tell the People Who Matter
📌 The Conversation Strategy
Deciding what to do after diagnosis includes figuring out who needs to know and when. This isn’t about shame or secrecy — it’s about timing and energy management, and it’s one of the trickier first steps after mental health diagnosis to navigate.
Start with your inner circle: the people who are most directly impacted by your well-being or who you know will be supportive. For me, that was my wife first, then gradually my older kids who were mature enough to understand.
Script for Close Family:
“I wanted to update you on something important. I’ve been struggling with [symptoms you’ve been experiencing], and I just got some answers from my doctor. I’ve been diagnosed with [condition], and I’m starting treatment. I’m telling you because you’re important to me, and I wanted you to know what’s going on.”
For Friends and Extended Family:
You don’t owe anyone a detailed explanation. A simple “I’m dealing with some health stuff and working with my doctor on treatment” is perfectly adequate. You can always share more later when you’re feeling more stable.
🔍 Managing Mental Health Stigma
Unfortunately, not everyone will respond with the same understanding they’d show if you were diagnosed with diabetes or high blood pressure. Some people still treat mental health conditions differently, and that’s their problem, not yours.
I’ve found that most negative reactions come from fear and misunderstanding rather than malice. People worry they’ll say the wrong thing, or they project their own fears about mental health onto your situation.
Don’t let other people’s discomfort dictate your healing journey. The people who truly matter will educate themselves and show up for you. The ones who don’t? They’ve shown you who they are. Protecting your energy during these first steps after mental health diagnosis is essential.
Avoiding the Dangerous Quick-Fix Trap
⚠️ Why “Just Think Positive” Doesn’t Work
In those early days after diagnosis, you’ll encounter well-meaning people offering solutions that sound simple but are actually harmful: “Just think positive thoughts,” “Have you tried yoga?” “Maybe you just need to get outside more.”
These suggestions aren’t necessarily wrong — positive thinking, yoga, and outdoor time can absolutely support mental health. But they’re not substitutes for professional treatment, and they can make you feel like you’re failing if they don’t magically cure your condition.
Managing mental health is like managing any chronic condition. You wouldn’t tell someone with diabetes to skip their insulin and just eat better. Mental health conditions often require a multi-faceted approach that includes professional support. Recognizing this truth is among the most important first steps after mental health diagnosis.
Red Flags to Avoid:
- Anyone promising to “cure” your mental health condition completely
- Expensive programs claiming to replace medical treatment
- Social media influencers selling courses on “healing naturally”
- Well-meaning friends insisting you don’t need medication
- Alternative treatments that require you to stop working with licensed professionals
💡 What Actually Helps in Early Recovery
Real mental health recovery tips focus on building sustainable habits and working with qualified professionals. Here’s what research and experience show actually makes a difference during the first steps after mental health diagnosis:
Stick to your treatment plan, even when you start feeling better. Many people discontinue therapy or medication once symptoms improve, which often leads to relapse.
Build routine slowly. Don’t try to overhaul your entire life in week one. Add one small positive habit at a time — maybe it’s taking a 10-minute walk or eating breakfast regularly.
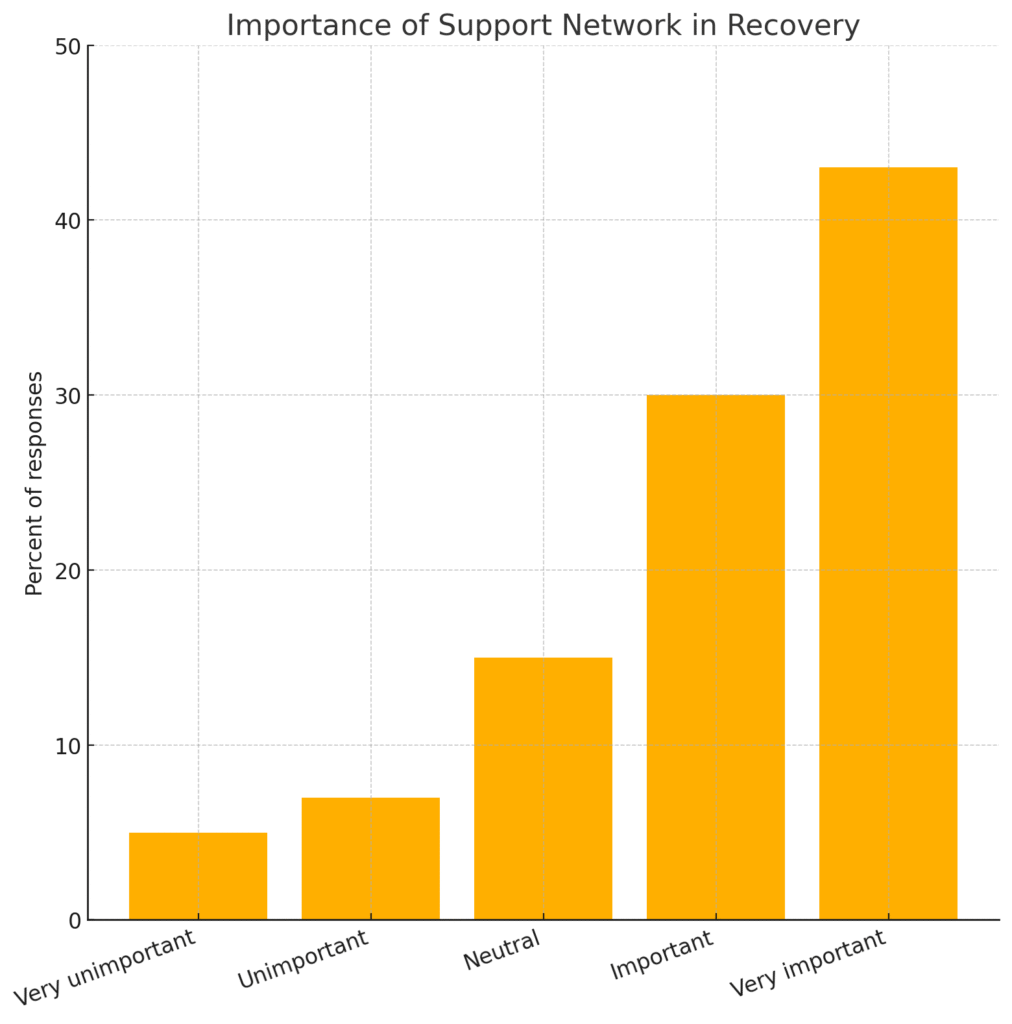
Connect with supportive people who understand mental health challenges. This might be a support group, online community, or friends who’ve been through similar experiences.
Building Your Treatment Team
🏥 Beyond Your Primary Doctor
Your diagnosis might have come from your family physician, but managing mental health often requires a team approach. Depending on your specific condition and needs, this team might include:
- Psychiatrist: Medical doctor specializing in mental health who can prescribe and monitor medications
- Therapist/Counselor: Licensed professional who provides talk therapy and coping strategies
- Social Worker: Can help connect you with community resources and support services
- Case Manager: Helps coordinate care between different providers
Don’t feel like you need to build this entire team in your first week. Start with one or two key players and expand as needed.
Questions to Ask Potential Providers:
What experience do you have treating my specific condition? How do you typically approach treatment? What should I expect in terms of timeline and progress? How do we measure whether treatment is working?
Good providers will welcome these questions and give you clear, honest answers. If someone seems evasive or makes promises that sound too good to be true, keep looking.
🔍 Insurance and Financial Planning
Mental health treatment is an investment in your future, but it shouldn’t bankrupt you. Most insurance plans are required to cover mental health services at the same level as physical health, but coverage varies widely.
Call your insurance company before your first appointments to understand your benefits. Ask about copays, deductibles, and whether you need referrals to see specialists.
If you’re uninsured or underinsured, community mental health centers often provide services on sliding fee scales. Many therapists also offer reduced rates for clients who need financial assistance.
Creating Your Daily Stability Framework

⚡ The Power of Micro-Routines
Those first weeks after diagnosis aren’t the time for dramatic lifestyle overhauls. Instead, focus on creating small, consistent routines that support your mental health without overwhelming your already-strained emotional resources.
I started with three micro-routines: making my bed every morning, eating something within an hour of waking up, and spending 10 minutes outside before noon. These weren’t cure-alls, but they gave me small wins to build on.
Morning Stability Anchors:
- Wake up at roughly the same time, even on weekends
- Have some form of protein within an hour of waking
- Limit news/social media consumption in the first hour
- Do one thing that makes you feel accomplished (make the bed, wash dishes, etc.)
Evening Wind-Down Protocol:
- Set a phone/screen curfew 30-60 minutes before bed
- Practice basic hygiene even when you don’t feel like it
- Prepare something for tomorrow (clothes, lunch, keys in the same spot)
- Write down one thing you’re grateful for or one thing that went okay that day
📌 Exercise and Mental Health Connection
Regular movement is one of the most effective tools for managing mental health conditions, but “exercise” doesn’t have to mean joining a gym or running marathons. Start where you are.
If you’re normally sedentary, walking for 10 minutes counts as exercise. If you’re already active, maintaining your current routine while your emotions stabilize is perfectly fine.
Research shows that even light exercise can be as effective as medication for some people with mild to moderate depression and anxiety. The key is consistency over intensity.
Low-Barrier Movement Options:
- Walking around your neighborhood or local mall
- YouTube yoga or stretching videos
- Dancing to music in your living room
- Gardening or yard work
- Playing actively with kids or pets
- Family fitness activities that include everyone
Medication: What to Expect and Why It Matters
💊 The Medication Reality Check
If medication was prescribed as part of your treatment plan, you probably have questions and concerns. This is completely normal — we’re talking about introducing chemicals that affect your brain chemistry.
Mental health medications aren’t “happy pills” that instantly fix everything. They’re tools that can help reduce symptoms enough for you to do the real work of recovery through therapy and lifestyle changes.
Most psychiatric medications take 4-8 weeks to reach full effectiveness. Some people notice improvements within days, others need several months to find the right medication and dosage. This process requires patience and close communication with your prescribing physician.
Common Early Side Effects to Expect:
- Mild nausea or stomach upset (usually improves with time)
- Changes in sleep patterns (temporary in most cases)
- Initial fatigue or drowsiness as your body adjusts
- Minor headaches during the first few weeks
- Appetite changes (increases or decreases)
Serious side effects are less common but require immediate medical attention. These include severe mood changes, thoughts of self-harm, extreme agitation, or unusual physical symptoms.
🧠 Working With Your Prescriber
Keep a simple medication log during your first month. Note when you take your medication, any side effects you experience, and any changes in your mood or symptoms. This information helps your doctor make adjustments if needed.
Never stop taking prescribed psychiatric medication suddenly, even if you feel better or don’t like the side effects. These medications often need to be tapered gradually to avoid withdrawal symptoms or relapse.
If you’re having problems with your current medication, schedule an appointment to discuss alternatives. There are usually multiple options within each class of psychiatric medications.
Building Long-Term Mental Health Resilience
🌟 Recovery Isn’t Linear
One of the most important things I wish someone had told me during those first steps after mental health diagnosis: recovery looks more like a zigzag than a straight line upward.
You’ll have good days and difficult days. You’ll make progress, then feel like you’re sliding backward. This isn’t failure — it’s the normal pattern of healing from mental health conditions.
Building resilience means developing the tools to navigate both the ups and downs with greater stability and confidence.
Long-Term Success Factors:
- Consistent treatment attendance: Even when you don’t feel like going
- Honest communication: With your treatment team about what’s working and what isn’t
- Lifestyle integration: Gradually building mental health support into your daily life
- Community connection: Maintaining relationships with supportive people
- Ongoing education: Learning about your condition and staying informed about new treatments
💡 When to Celebrate Progress
Progress in mental health recovery often happens in small increments that are easy to miss if you’re only looking for dramatic changes. Celebrate the small wins:
- Going a full week without missing medications
- Having a difficult conversation without shutting down
- Asking for help when you need it
- Getting through a trigger situation using healthy coping skills
- Maintaining your treatment appointments consistently
Professional vs. Peer Support: Both Matter
👥 The Power of Shared Experience
Professional treatment provides the clinical expertise and evidence-based interventions you need for recovery. But peer support — connecting with others who’ve walked similar paths — offers something different and equally valuable.
Support groups, whether in-person or online, can help you feel less isolated in your experience. Hearing how others have navigated similar challenges can provide hope and practical strategies.
The National Alliance on Mental Illness (NAMI) offers both in-person and virtual support groups for people with mental health conditions and their families.
Finding the Right Support Community:
- Look for groups that focus on your specific diagnosis
- Choose facilitated groups over purely social forums
- Pay attention to whether discussions are solution-focused or primarily complaint-focused
- Consider both in-person and online options to find what works for your schedule
- Don’t be afraid to try several groups before finding the right fit
🔍 Red Flags in Support Communities
Not all peer support is helpful. Avoid communities that:
- Discourage professional treatment or medication
- Focus primarily on sharing trauma stories without coping strategies
- Allow members to provide medical advice or diagnose others
- Create drama or become toxic social environments
- Push specific products, treatments, or belief systems
Protecting Your Recovery Investment
📌 Creating Boundaries for Your Healing
Mental health recovery requires protecting your emotional energy and time. This means learning to say no to commitments that drain you and yes to activities that support your wellbeing.
You don’t owe anyone an explanation for prioritizing your mental health. Taking care of yourself isn’t selfish — it’s essential for being able to show up for the people and responsibilities that matter most to you.
Practical Boundary Setting:
- Limit exposure to negative news or social media if it worsens your symptoms
- Reduce time with people who are consistently draining or unsupportive
- Say no to optional commitments during your early recovery period
- Ask family members to respect your treatment schedule and self-care time
- Set limits on discussing your diagnosis with people who aren’t helpful
⚡ Managing Setbacks and Relapses
Mental health conditions are often chronic, which means symptoms can return even during successful treatment. This doesn’t mean treatment isn’t working or that you’re doing something wrong.
Having a setback plan can help you respond quickly and effectively when symptoms return:
- Know the early warning signs specific to your condition
- Have a list of people to call when you need extra support
- Keep contact information for your treatment providers easily accessible
- Maintain a basic self-care toolkit (comfort items, coping strategies, etc.)
- Know when to seek immediate help versus when to wait for your next regular appointment
The Reality About Mental Health and Family Life
👨👩👧👦 How Diagnosis Affects Family Dynamics
If you have a spouse and children, your mental health diagnosis doesn’t just affect you — it impacts your entire family system. This can feel overwhelming, but it can also be an opportunity to model healthy coping and help reduce mental health stigma for the next generation.
Kids are remarkably perceptive. They often know something is different even if you haven’t told them about your diagnosis. Age-appropriate honesty is usually better than trying to hide everything.
Talking to Children About Your Mental Health:
- Young children (5-8): “Daddy’s brain works a little differently sometimes, and I’m learning new ways to help it feel better.”
- Tweens (9-12): “I’ve been struggling with anxiety/depression, and I’m working with doctors to manage it better.”
- Teens (13+): More detailed conversation about the specific condition, treatment, and how it might affect family life
🏠 Creating a Mentally Healthy Home Environment
Your recovery doesn’t happen in isolation — it happens within the context of your daily life. Making your home environment more supportive of mental health benefits everyone in the family.
This might mean establishing quieter morning routines, creating spaces where family members can decompress, or implementing technology boundaries that support better sleep and connection.
Family Mental Health Practices:
- Regular family meetings to check in on everyone’s wellbeing
- Normalize talking about feelings and emotions
- Practice gratitude or mindfulness activities together
- Maintain consistent routines that provide stability
- Model healthy conflict resolution
- Create traditions that bring joy and connection
Financial Planning for Mental Health Care
💰 The Long-Term Investment Perspective
Mental health treatment is an investment that pays dividends for years to come. However, the upfront costs can feel overwhelming, especially if you’re dealing with reduced work capacity due to your symptoms.
Most mental health conditions benefit from both short-term intensive treatment and long-term maintenance care. Planning for both phases can help you make informed decisions about your care.
Typical Cost Considerations:
- Initial psychiatric evaluation: $300-800
- Ongoing therapy sessions: $100-250 per session
- Psychiatric medication management: $200-400 per visit
- Prescription medications: $20-500+ per month depending on insurance
- Potential intensive programs: $1000-10,000+ for specialized treatment
Money-Saving Strategies:
- Utilize employee assistance programs (EAP) through your workplace
- Look for therapists who offer sliding fee scales
- Consider group therapy, which is often less expensive than individual sessions
- Ask about payment plans with providers
- Research pharmaceutical assistance programs for expensive medications
- Use community mental health centers for more affordable options
Technology and Mental Health Recovery
📱 Digital Tools That Actually Help
While social media and constant connectivity can worsen mental health symptoms, the right technology can support your recovery when used intentionally.
Mental health apps aren’t replacements for professional treatment, but they can supplement your care and provide support between appointments.
Evidence-Based App Categories:
- Mood tracking: Help identify patterns in symptoms and triggers
- Meditation/mindfulness: Guided practices for stress reduction and emotional regulation
- CBT tools: Interactive exercises based on cognitive behavioral therapy principles
- Crisis support: Quick access to hotlines and coping strategies during difficult moments
- Medication reminders: Help maintain consistency with prescribed treatments
🧠 Digital Boundaries for Mental Health
Part of managing mental health in 2025 means being intentional about your relationship with technology. Constant notifications, negative news cycles, and social comparison can exacerbate symptoms of anxiety and depression.
Consider implementing “digital hygiene” practices:
- Morning phone-free time to start your day with intention
- News consumption limits to prevent information overload
- Social media boundaries, including unfollowing accounts that consistently make you feel worse
- Evening screen curfews to protect sleep quality
- Regular “digital detox” periods to reconnect with offline activities and relationships
Moving Forward: Your Next 30 Days
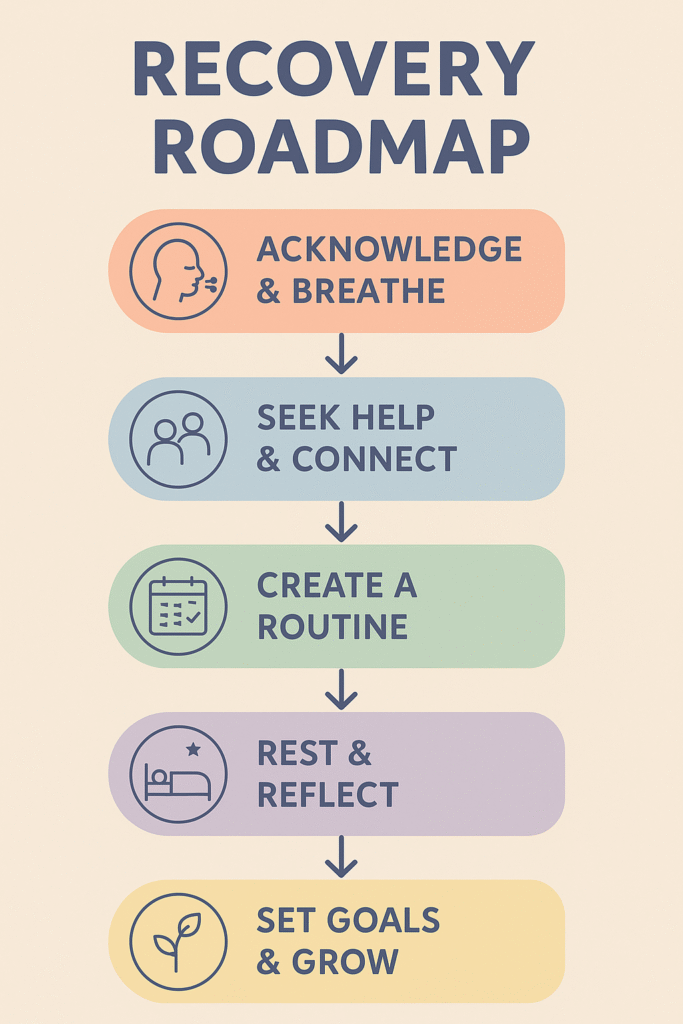
🎯 Week 1 Priorities
Your first week should focus on stability and information gathering. Don’t try to fix everything immediately — just focus on getting your bearings and ensuring you’re safe.
- Attend all scheduled medical appointments
- Fill prescriptions if medication was prescribed
- Identify 2-3 people in your support network
- Establish basic daily routines (sleep, meals, hygiene)
- Limit major life decisions or changes
Week 2-3 Goals
As you start to stabilize, you can begin implementing slightly more structure and reaching out for additional support.
- Research and contact potential therapists if therapy was recommended
- Join a support group or online community
- Begin gentle, consistent movement/exercise
- Start tracking your mood and symptoms
- Have initial conversations with close family members or friends
Week 4 and Beyond
By the end of your first month, you should have the beginnings of a treatment plan and support system in place.
- Evaluate how your initial treatment is working
- Make any necessary adjustments to medications with your doctor
- Establish longer-term therapy goals
- Begin implementing lifestyle changes that support mental health
- Plan for ongoing recovery and setback prevention
Living Authentically With Mental Health Conditions
💪 Redefining Strength
Society often portrays mental health struggles as weakness, but I’ve learned the opposite is true. It takes tremendous courage to face your mental health challenges head-on and commit to treatment.
Seeking help isn’t giving up — it’s fighting for your life, relationships, and future. Every therapy appointment, every dose of medication, every day you choose healthy coping strategies over harmful ones is an act of strength.
What Recovery Really Looks Like
Recovery doesn’t mean you’ll never have symptoms again. It means you’ll have better tools for managing symptoms when they arise, more support to help you through difficult periods, and greater self-awareness about what works for your mental health.
For some people, recovery means returning to their previous level of functioning. For others, it means finding new ways to thrive that account for their mental health needs. Both paths are valid.
🌟 Hope for Your Future
I’m writing this five years after my initial diagnosis, and while I still manage symptoms of PTSD and anxiety, my life is fuller and richer than it was before I got help. Treatment didn’t just address my symptoms — it gave me tools for handling life’s challenges that I never had before.
Your diagnosis isn’t the end of your story. It’s the beginning of a new chapter where you have more information, better tools, and professional support for navigating life’s ups and downs.
Mental health recovery is possible. It takes time, effort, and often patience with the process. But the investment you’re making in your mental health today will pay dividends for years to come.
The first steps after mental health diagnosis might feel overwhelming right now, but you don’t have to take them alone. Professional help is available, effective treatments exist, and millions of people have walked this path before you and gone on to live meaningful, fulfilling lives.
Your journey is just beginning, and you have every reason to be hopeful about what lies ahead.
Explore More from Our Family of Blogs
Mountains Will Move
Faith-based encouragement for everyday families.
Everyday Exposed
No-filter truth hub for critical thinking and clarity.
Thank you for being part of the community. God Bless you and your family.