7 Bipolar Disorder Secrets: Ultimate Mental Health Guide 🧠
Mental health conversations have changed dramatically in our household over the past twenty years. As a father raising six kids with my wife who’s spent her career in education, we’ve seen firsthand how mental health conditions affect not just individuals, but entire families.
Bipolar disorder stands out as one of the most misunderstood and complex mental health conditions. The extreme mood swings from euphoric highs to devastating lows create a rollercoaster that impacts everyone in the family orbit.
Understanding this condition isn’t just about medical knowledge—it’s about recognizing the human experience behind the diagnosis. Whether you’re supporting a family member, seeking answers for yourself, or simply want to understand mental health better, this comprehensive guide breaks down everything you need to know about bipolar disorder.
What Is Bipolar Disorder? The Reality Behind the Name 📊
Bipolar disorder affects millions of people worldwide, yet many still think it’s simply “mood swings” or being “moody.” That couldn’t be further from the truth.
This chronic mental health condition involves extreme shifts between manic episodes (abnormally elevated mood) and depressive episodes (intense sadness or hopelessness). These aren’t ordinary ups and downs—they’re dramatic changes that significantly impair daily functioning.
The condition was previously called manic-depressive illness, which actually describes it more accurately. During my Air Force years, I witnessed service members struggle with undiagnosed bipolar disorder, often leading to career-ending situations that could have been prevented with proper understanding and treatment.
What makes bipolar disorder particularly challenging is its unpredictable nature. Episodes can last days, weeks, or even months. Between episodes, many people function completely normally, which sometimes leads to delayed diagnosis or misunderstanding from others.
The statistics surrounding this condition are sobering. According to the National Institute of Mental Health, approximately 2.8% of U.S. adults experience bipolar disorder in any given year, with nearly 83% of cases classified as severe.
The Science Behind Bipolar Disorder: What Causes This Complex Condition? 🔬
Understanding the causes of bipolar disorder helps remove stigma and blame. This isn’t something people choose or bring upon themselves through poor decisions.
Genetic Factors: The Family Connection
Research consistently shows that genetics play a significant role in bipolar disorder development. If you have a parent or sibling with the condition, your risk increases substantially.
Recent genome-wide association studies have identified specific genes like ANK3, CACNA1C, and ODZ4 that influence neuronal functioning and calcium channel regulation. These findings from Harvard Medical School suggest that multiple genes contribute to bipolar disorder risk rather than a single “bipolar gene.”
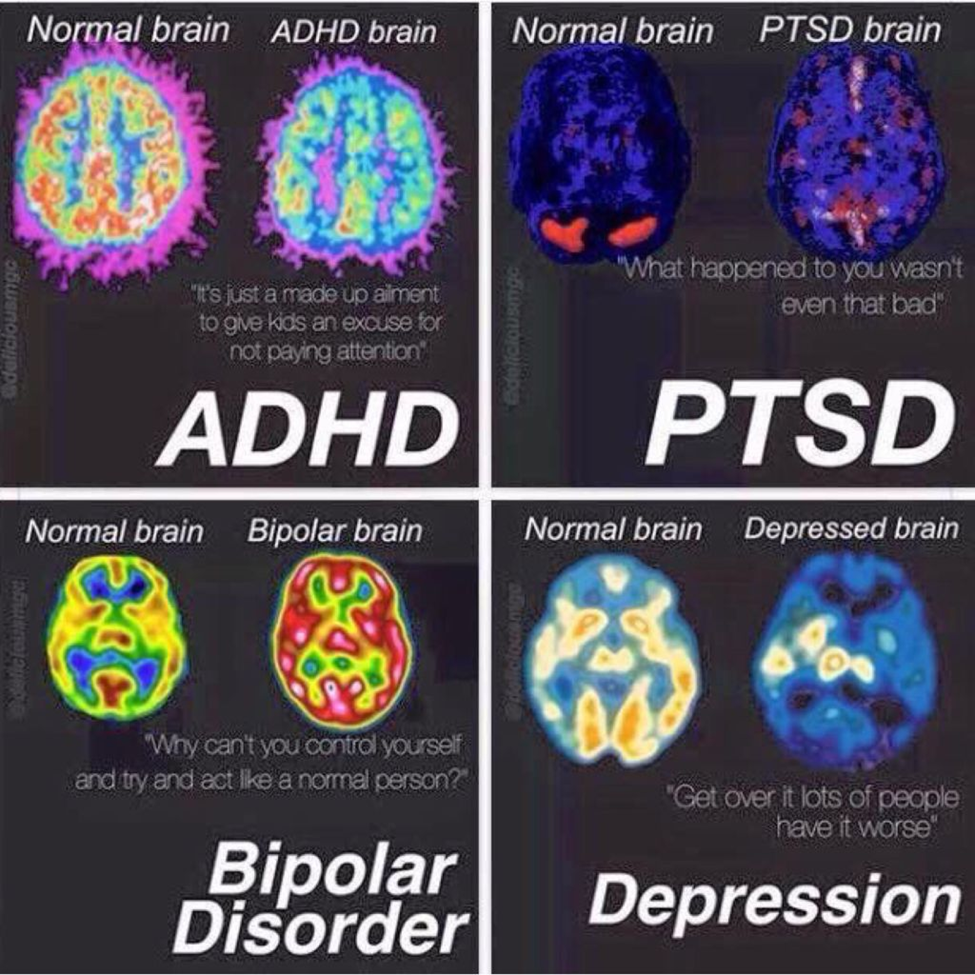
Brain Structure and Function
Advanced neuroimaging reveals fascinating differences in bipolar brains. MRI studies show alterations in the prefrontal cortex, amygdala, hippocampus, and striatum—regions crucial for emotional regulation and decision-making.
The neurotransmitter systems also function differently. Dopamine, serotonin, and glutamate—the brain’s chemical messengers—don’t communicate normally in people with bipolar disorder. This explains why medications targeting these systems can be so effective.
Environmental Triggers
While genetics load the gun, environment pulls the trigger. Childhood trauma, significant stress, substance abuse, and disrupted sleep patterns can all trigger the onset of bipolar disorder in genetically vulnerable individuals.
Interestingly, research from Johns Hopkins shows that even viral infections during pregnancy might increase bipolar disorder risk in offspring.
Types of Bipolar Disorder: Not All Cases Are the Same 📋
The types of bipolar disorder vary significantly in severity and presentation. Understanding these differences is crucial for proper treatment and family support.
Photo from ScienceDirect
Bipolar I Disorder: The Full Spectrum
Bipolar I disorder represents the classic form most people imagine. It requires at least one full manic episode lasting seven days or severe enough to require hospitalization.
These manic episodes are intense. I’ve seen military personnel go from model soldiers to making catastrophically poor decisions within days during manic episodes. The person might feel invincible, need minimal sleep, spend money recklessly, or engage in dangerous behaviors.
Depressive episodes often follow, but they’re not required for a Bipolar I diagnosis. However, most people with Bipolar I experience both extremes.
Bipolar II Disorder: The Subtle Distinction
Bipolar II disorder involves hypomanic episodes rather than full mania, plus at least one major depressive episode. Hypomania is like mania’s quieter cousin—elevated mood and energy, but not severe enough to cause major impairment.
This subtlety makes Bipolar II tricky to diagnose. People might seem especially productive or creative during hypomanic periods, leading others to miss the warning signs.
Cyclothymic Disorder: The Persistent Pattern
Cyclothymic disorder involves numerous periods of hypomanic and depressive symptoms over at least two years (one year in children). These symptoms don’t meet the full criteria for major episodes but create persistent instability.
Think of it as bipolar disorder’s milder but persistent cousin. The mood swings are less dramatic but more constant, creating ongoing challenges in relationships and daily functioning.
Recognizing Bipolar Symptoms: The Warning Signs That Matter ⚠️
Bipolar symptoms manifest differently during manic and depressive episodes. Recognizing these patterns can be lifesaving for families.
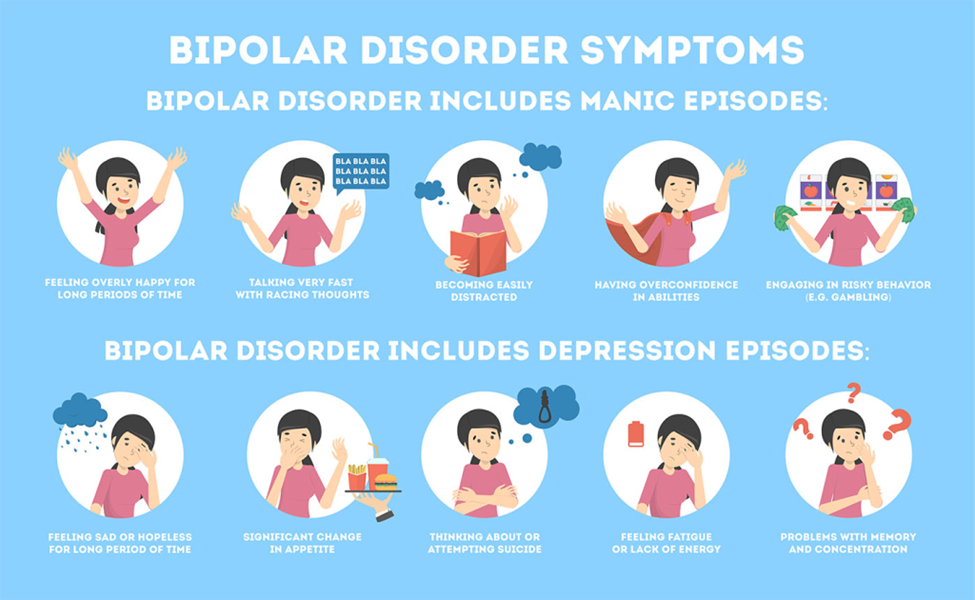
Manic Episode Symptoms
During manic episodes, people experience:
Elevated mood and energy that seems almost superhuman. They might feel euphoric, extremely optimistic, or intensely irritable without clear cause.
Decreased need for sleep becomes dramatic—functioning on 2-3 hours nightly for days or weeks without feeling tired.
Racing thoughts and rapid speech make conversations difficult to follow. Ideas jump from topic to topic without logical connections.
Poor judgment and risky behaviors emerge suddenly. This might include excessive spending, sexual indiscretions, business investments, or dangerous driving.
Grandiose beliefs about abilities or importance can lead to unrealistic plans or claims of special powers or connections.
Depressive Episode Symptoms
Depressive episodes in bipolar disorder often feel more severe than regular depression:
Persistent sadness or emptiness that doesn’t respond to positive events or good news.
Loss of interest in previously enjoyed activities, including hobbies, sex, or social connections.
Significant changes in appetite and sleep patterns—either too much or too little of both.
Fatigue and low energy make simple tasks feel overwhelming.
Feelings of worthlessness or excessive guilt about past events or imagined failures.
Suicidal thoughts or behaviors require immediate professional intervention.
Mixed Episodes: The Dangerous Combination
Some people experience mixed episodes with symptoms of both mania and depression simultaneously. These episodes are particularly dangerous because the energy of mania combines with the hopelessness of depression, significantly increasing suicide risk.
Diagnosing Bipolar Disorder: The Path to Understanding 🩺
Bipolar disorder diagnosis requires comprehensive psychiatric evaluation by qualified mental health professionals. There’s no simple blood test or brain scan—diagnosis relies on careful observation of symptoms and patterns.
The DSM-5 Criteria
Mental health professionals use the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) for accurate bipolar diagnosis. These criteria specify exactly what constitutes manic, hypomanic, and depressive episodes.
For Bipolar I diagnosis, one manic episode is sufficient. For Bipolar II diagnosis, both hypomanic and depressive episodes must occur. The timing, duration, and severity of symptoms all matter.
Assessment Tools and Rating Scales
Clinicians use various mood assessment tools to track symptoms over time. The Young Mania Rating Scale (YMRS) measures manic symptoms, while the Hamilton Depression Rating Scale assesses depressive symptoms.
These tools help monitor treatment progress and identify patterns that might predict episode onset.
Photo from DrugWatch
The Importance of Accurate Diagnosis
Misdiagnosis happens frequently with bipolar disorder. It’s often confused with major depression, ADHD, or personality disorders.
Getting the right diagnosis matters enormously. Treatment for unipolar depression can actually trigger manic episodes in people with bipolar disorder, making accurate identification crucial.
Treatment Options: Building a Path to Stability 💊
Photo from VeryWellMind
Bipolar disorder treatment typically involves multiple approaches working together. No single intervention works for everyone, and finding the right combination takes time and patience.
Medication Management

Mood stabilizers form the foundation of most treatment plans. Lithium remains the gold standard—it’s been used for decades and has extensive research supporting its effectiveness for both manic and depressive episodes.
Anticonvulsants like valproate and lamotrigine also stabilize mood effectively. These medications were originally developed for epilepsy but prove excellent for bipolar disorder.
Antipsychotic medications help control severe manic or mixed episodes. Newer atypical antipsychotics like quetiapine and aripiprazole have fewer side effects than older versions.
Antidepressants require careful use in bipolar disorder. They’re sometimes necessary for severe depression but must be combined with mood stabilizers to prevent triggering mania.
Psychotherapy Approaches
Photo from Indiana Center for Recovery
Cognitive Behavioral Therapy (CBT) helps people identify thought patterns and behaviors that contribute to mood episodes. It’s particularly effective for developing coping strategies and preventing relapse.
Interpersonal and Social Rhythm Therapy (IPSRT) focuses on maintaining regular daily routines and improving relationship skills. Since disrupted sleep and social stress often trigger episodes, this approach addresses key vulnerability factors.
Family-Focused Therapy (FFT) involves family members in treatment. As someone who’s navigated family challenges with six kids, I can’t overstate how important family support becomes in mental health recovery.
Lifestyle Modifications
Sleep hygiene becomes absolutely critical for people with bipolar disorder. Disrupted sleep can trigger episodes faster than almost anything else.
Regular exercise provides natural mood stabilization. Research from Mayo Clinic shows that consistent physical activity reduces both manic and depressive symptoms.
Stress management techniques like meditation, yoga, or deep breathing help prevent episode triggers. Learning to recognize and manage stress becomes a crucial life skill.
Avoiding alcohol and drugs is essential. Substance use dramatically increases episode frequency and severity while interfering with medication effectiveness.
Photo from Research Gate
Impact on Families: The Ripple Effects of Bipolar Disorder 👨👩👧👦
Photo from Unsplash
Bipolar disorder affects families in ways that extend far beyond the diagnosed individual. Having raised six children, I’ve seen how one family member’s mental health challenges influence everyone’s daily life.
Relationship Strain and Communication Challenges
Family relationships often suffer during mood episodes. Manic behavior can feel exciting initially but becomes exhausting and frightening. The person might make promises they can’t keep, spend money the family doesn’t have, or behave in ways that embarrass or worry other family members.
Depressive episodes bring different challenges. The person might withdraw completely, unable to participate in family activities or fulfill their usual responsibilities. Children especially struggle to understand why mom or dad suddenly can’t get out of bed or seems uninterested in things they previously enjoyed.
Communication becomes complicated when you’re never sure which version of your family member you’ll encounter on any given day.
Financial and Practical Consequences
Economic impact often accompanies bipolar disorder. Manic episodes can lead to impulsive purchases, risky investments, or job loss due to inappropriate behavior. Depressive episodes might result in missed work or inability to maintain employment.
These financial stresses compound family tension, especially when medical bills and therapy costs add to existing pressures.
Children’s Adjustment and Understanding
Children in bipolar families need special support and age-appropriate explanations. They might blame themselves for a parent’s mood changes or feel responsible for “fixing” the situation.
Research shows that children of parents with bipolar disorder have higher rates of mental health issues themselves, making early intervention and family support crucial.
Building Family Resilience
Successful families learn to separate the person from the disorder. They develop crisis plans, recognize warning signs, and create supportive environments that promote stability.
Family routines become even more important when someone has bipolar disorder. Predictable schedules help everyone feel more secure and can help prevent episode triggers.
Living Successfully with Bipolar Disorder: Practical Strategies 🌟
Managing bipolar disorder requires developing a comprehensive toolkit of strategies that work during both stable periods and mood episodes.
Creating Effective Daily Routines
Routine becomes medicine for people with bipolar disorder. Regular sleep, meal times, exercise, and activities help maintain mood stability.
This doesn’t mean rigid schedules that create stress. Instead, it means consistent patterns that support mental health while allowing for life’s natural variations.
Building Your Support Network
Strong support systems make enormous differences in long-term outcomes. This includes family, friends, healthcare providers, and peer support groups.
The National Alliance on Mental Illness (NAMI) offers excellent resources for both individuals and families dealing with bipolar disorder.
Developing Crisis Management Plans
Crisis planning involves identifying early warning signs and creating specific action steps for different scenarios. This might include emergency contacts, medication adjustments, or hospitalization criteria.
Having plans in place before crisis hits reduces panic and ensures faster, more effective responses.
Maintaining Treatment Adherence
Medication compliance remains one of the biggest challenges in bipolar treatment. People often discontinue medications during stable periods or when side effects become bothersome.
Working closely with healthcare providers to find the right medication balance and understanding the importance of consistent treatment helps prevent relapses.
Stress Management and Self-Care
Photo from Psych Central
Stress reduction techniques become essential life skills. This might include regular exercise, meditation, hobbies, or creative outlets.
Learning to recognize personal stress triggers and developing healthy coping mechanisms helps prevent episodes before they start.
Professional Help and Resources: Finding the Right Support 🔍
Getting professional help for bipolar disorder requires finding qualified mental health providers who understand the complexity of this condition.
Types of Mental Health Professionals
Psychiatrists can diagnose bipolar disorder and prescribe medications. They’re medical doctors who specialize in mental health conditions.
Psychologists provide therapy and psychological testing but typically can’t prescribe medications (except in a few states).
Licensed clinical social workers and professional counselors offer therapy and case management services.
Peer support specialists have lived experience with mental health conditions and provide unique insights and support.
Finding Quality Care
Insurance coverage for mental health treatment has improved significantly, but finding providers who accept insurance can still be challenging.
The Substance Abuse and Mental Health Services Administration (SAMHSA) provides a national helpline and treatment locator service.
Many communities have community mental health centers that provide services regardless of ability to pay.
Emergency Resources
Crisis situations require immediate professional intervention. The National Suicide Prevention Lifeline (988) provides 24/7 support for people in crisis.
Most communities have mobile crisis teams that can respond to homes during psychiatric emergencies.
Emergency departments at hospitals can provide immediate safety and stabilization during severe episodes.
Hope and Recovery: The Long-Term Outlook 🌈
Recovery from bipolar disorder doesn’t mean cure—it means learning to manage the condition effectively while living a fulfilling life.
Success Stories and Realistic Expectations
Many people with bipolar disorder live successful lives with proper treatment and support. They maintain careers, relationships, and families while managing their mental health.
Recovery looks different for everyone. Some people experience long periods of stability with occasional episodes, while others require more intensive ongoing management.
The Importance of Early Intervention
Early diagnosis and treatment significantly improve long-term outcomes. The sooner people receive appropriate care, the better their chances of maintaining stability and preventing severe episodes.
Ongoing Management and Monitoring
Lifelong management typically involves regular psychiatric appointments, medication monitoring, therapy sessions, and lifestyle maintenance.
This ongoing commitment to mental health becomes part of daily life, much like managing diabetes or other chronic conditions.
Research and Future Developments
Current research continues exploring new medications, therapy approaches, and even genetic testing to predict medication responses.
Brain stimulation therapies like transcranial magnetic stimulation (TMS) show promise for treatment-resistant cases.
Digital health tools and smartphone apps are being developed to help people track moods, medications, and warning signs more effectively.
Moving Forward with Understanding and Compassion 💝
Bipolar disorder remains one of the most challenging mental health conditions for individuals and families. The extreme mood swings, unpredictable episodes, and long-term management requirements create ongoing stress and uncertainty.
Yet with proper understanding, treatment, and support, people with bipolar disorder can lead meaningful, productive lives. The key lies in education, early intervention, consistent treatment, and strong support systems.
As families, we must remember that mental health conditions don’t define people—they’re challenges to manage, not character flaws to fix. The person you love remains the same individual, even when their brain chemistry creates difficulties.
The journey with bipolar disorder requires patience, understanding, and hope. Some days will be harder than others, but with the right tools and support, stability and happiness are achievable goals.
Whether you’re supporting a family member, seeking help for yourself, or simply wanting to understand mental health better, remember that knowledge creates power, and understanding builds compassion.
Mental health matters for every family member. By approaching these challenges with education, empathy, and appropriate professional support, we can create environments where everyone has the opportunity to thrive.
🌐 Explore More from Our Family of Blogs
If you found this article helpful, you might also enjoy what we’re sharing across our other platforms. Each one is designed to uplift, equip, and inspire families in real, practical ways:
🏠 Mountains Will Move
Faith-based encouragement for everyday families. We dive into prayer, parenting, purpose, and pressing through life’s hardest seasons with Jesus at the center.
👉 Visit Mountains Will Move »
🔎 Everyday Exposed
Our no-filter truth hub—where we tackle myths, challenge misleading narratives, and bring clarity to the conversations that matter most.
👉 Visit Everyday Exposed »
Whether you’re diving deeper into pet care, faith, or uncovering truth in today’s noisy world, I hope you’ll journey with us.
Thank you for being part of the community. God Bless you and your family. 🙏