5 Evidence-Based Trauma Recovery Strategies That Actually Work
You’re not broken. You’re not weak. And you’re definitely not alone.
As a father of six kids (five girls and one boy) and an Air Force veteran married for over two decades, I’ve witnessed trauma’s impact firsthand—both in military service and in helping my family navigate life’s unexpected challenges. My wife, a middle school math teacher, often reminds me that healing isn’t a linear equation—there’s no simple formula that works for everyone.
But here’s what I’ve learned through personal experience, professional research, and countless conversations with fellow veterans and families: trauma recovery is absolutely possible when you have the right strategies and support system in place.
Understanding Trauma Recovery: More Than Just “Getting Over It” 💪
Trauma recovery isn’t about forgetting what happened or pretending everything’s fine. It’s about reclaiming your power, rebuilding your sense of safety, and developing the tools to live fully despite what you’ve experienced.
Emotional healing requires both courage and patience. After serving in the Air Force, I’ve seen too many good people struggle in silence, thinking they should just “tough it out.” That’s not healing—that’s surviving. And you deserve more than survival.
The truth is, trauma therapy and evidence-based trauma treatment methods have advanced significantly. We now understand that healing happens when we address trauma from multiple angles: mentally, physically, emotionally, and spiritually.
The Science Behind Effective Trauma Recovery
Recent advances in neuroscience have revolutionized our understanding of how trauma affects the brain. According to research published in the Journal of Traumatic Stress, trauma literally changes brain structure, but the good news? Our brains are remarkably adaptable.
Neuroplasticity—the brain’s ability to reorganize and form new neural connections—means that healing is possible at any age. This scientific foundation gives us hope and validates what many trauma survivors instinctively know: with the right approach, things can get better.
Strategy #1: Build Your Support Network (It’s Not Optional) 🤝
Seeking support from your social circle isn’t just helpful—it’s essential for trauma recovery. I learned this lesson the hard way during my military service when I tried to handle everything alone.
Here’s the reality: isolation feeds trauma. When we withdraw from others, we give our traumatic experiences more power over our lives. Research from Ozbay et al. (2007) consistently shows that social support directly impacts mental health and recovery outcomes.

Creating Your Support Circle
Your support network doesn’t need to be huge, but it needs to be genuine. Consider these options:
Family members who understand and respect your healing journey can provide consistent emotional anchoring. My wife has been instrumental in my own healing process, offering both patience and accountability when I needed it most.
Close friends who’ve earned your trust create safe spaces where you can be authentically yourself without judgment. These relationships remind you that you’re valued beyond your trauma.
Support groups connect you with others who truly understand your experience. Whether it’s veterans’ groups, trauma survivors’ networks, or faith-based communities, shared understanding accelerates healing.
Professional counselors provide expert guidance and evidence-based techniques. There’s no shame in seeking professional help—it’s actually one of the smartest decisions you can make for your emotional healing.
The Power of Vulnerability
Sharing your story doesn’t mean oversharing with everyone. It means finding safe people and safe spaces where you can be honest about your struggles and victories. This vulnerability creates connection, and connection counters trauma’s isolating effects.
Research from the University of California demonstrates that social connection actually changes our brain chemistry, reducing stress hormones and increasing feel-good neurotransmitters like oxytocin and serotonin.
Strategy #2: Master Mindfulness and Relaxation Techniques 🧘♂️
Mindfulness-based interventions have revolutionized trauma treatment, and for good reason. When trauma hijacks your nervous system, mindfulness helps you regain control.
Lindahl et al. (2017) proved that mindfulness practices significantly reduce trauma-related distress and improve overall well-being. But let me be straight with you—this isn’t about sitting cross-legged chanting “om” (unless that works for you).

Practical Mindfulness for Real People
Breathing exercises can be done anywhere, anytime. When my youngest daughter had nightmares after a car accident, we practiced the “4-7-8 technique” together: inhale for 4 counts, hold for 7, exhale for 8. Simple, effective, and backed by science from Harvard Medical School.
Progressive muscle relaxation helps you identify and release physical tension that trauma creates in your body. Start with your toes and work your way up, tensing each muscle group for 5 seconds, then releasing.
Grounding techniques anchor you in the present moment when flashbacks or anxiety threaten to overwhelm you. The “5-4-3-2-1 technique” engages your senses: identify 5 things you can see, 4 you can touch, 3 you can hear, 2 you can smell, and 1 you can taste.
Building Mindfulness Into Daily Life
You don’t need hours of meditation to benefit from mindfulness. Research by Hoge et al. (2013) shows that even brief mindfulness practices reduce anxiety and promote emotional regulation.
Mindful eating turns meals into healing opportunities. Pay attention to flavors, textures, and your body’s hunger and fullness cues.
Walking meditation combines physical movement with present-moment awareness. As someone who spent years in military formations, I appreciate that healing can happen while moving forward—literally and figuratively.
For more practical strategies on developing positive mindset habits that support your healing journey, these evidence-based approaches can transform your daily experience.
Strategy #3: Exercise Your Way to Emotional Freedom 🏃♂️
Physical exercise isn’t just good for your body—it’s medicine for your traumatized mind and spirit. The connection between physical activity and emotional healing is so strong that some therapists now prescribe exercise alongside traditional therapy.
Stathopoulou et al. (2006) and Cooney et al. (2013) provide compelling evidence that consistent physical activity reduces depression, anxiety, and stress symptoms. But as a father juggling six kids’ schedules, I know finding time for exercise can feel impossible.

Exercise That Fits Real Life
High-intensity interval training (HIIT) delivers maximum mental health benefits in minimal time. Even 15 minutes of intense exercise releases endorphins—your brain’s natural mood elevators.
Strength training builds both physical and emotional resilience. There’s something powerful about proving to yourself that you’re stronger than you thought. Research from the Journal of Clinical Psychiatry shows that resistance training significantly reduces anxiety symptoms.
Outdoor activities combine exercise with nature therapy. Whether it’s hiking, gardening, or playing catch with your kids, outdoor movement provides additional mental health benefits through sunlight exposure and fresh air.
Creating Your Exercise Strategy
Start small but start consistently. Trauma recovery benefits more from regular, moderate exercise than sporadic intense workouts that leave you exhausted and discouraged.
Morning movement sets a positive tone for your entire day. Even 10 minutes of stretching or walking can shift your nervous system from reactive to responsive.
Family-friendly fitness kills two birds with one stone—you get exercise while modeling healthy habits for your children. Bike rides, dance parties in the living room, or backyard games create connection while promoting healing.
The key is finding activities you actually enjoy. Exercise shouldn’t feel like punishment—it should feel like self-care and empowerment.
Strategy #4: Rewire Your Thinking With Cognitive Behavioral Techniques 🧠
Cognitive Behavioral Therapy (CBT) remains the gold standard for trauma treatment because it addresses the thought patterns that keep you stuck in survival mode. Resick et al. (2002) and Bradley et al. (2005) demonstrate CBT’s effectiveness in helping people reframe traumatic experiences and develop healthier coping strategies.
But you don’t need to wait for a therapy appointment to start implementing CBT principles in your daily life.
Understanding the Trauma-Thought Connection
Trauma doesn’t just affect what you remember—it changes how you think about yourself, others, and the future. Common trauma-related thought patterns include:
All-or-nothing thinking: “I’m completely safe or in total danger.” Catastrophizing: “If something bad happened before, it will definitely happen again.” Self-blame: “I should have done something different to prevent this.” Hypervigilance: “I must constantly watch for threats.”
These thought patterns made sense during your traumatic experience—they helped you survive. But continuing to think this way can prevent healing and keep you trapped in the past.
Practical CBT Techniques for Daily Use
Thought challenging involves questioning the accuracy and helpfulness of trauma-related thoughts. When you notice catastrophic thinking, ask yourself: “Is this thought based in current reality or past trauma? What evidence supports or contradicts this thought?”
Behavioral experiments help you test trauma-related beliefs in safe, controlled ways. If trauma has made you afraid of crowded places, you might start by spending 5 minutes in a small group, gradually building tolerance and confidence.
Cognitive restructuring involves replacing unhelpful thoughts with more balanced, realistic ones. Instead of “I can’t handle this,” try “This is challenging, but I have tools and support to get through it.”
Building New Mental Habits
Remember, your brain learned trauma responses through repetition—it will learn healthier responses the same way. Research from UCLA shows that it takes consistent practice over time to create new neural pathways.
Daily thought logs help you identify patterns and track progress. Simply noting your emotions and the thoughts that triggered them increases self-awareness and emotional regulation.
Positive self-talk isn’t about toxic positivity—it’s about treating yourself with the same compassion you’d show a good friend facing similar challenges.
For additional strategies on maintaining mental and emotional well-being, explore these comprehensive health and well-being strategies that complement trauma recovery work.
Strategy #5: Seek Professional Trauma Therapy (You’re Worth the Investment) 💼
If you’re struggling with trauma, seeking professional help isn’t admitting defeat—it’s choosing victory. As a veteran myself, I understand the stigma around mental health treatment, especially in military and traditional communities. But here’s the truth: trauma therapy works, and you deserve access to the best possible care.
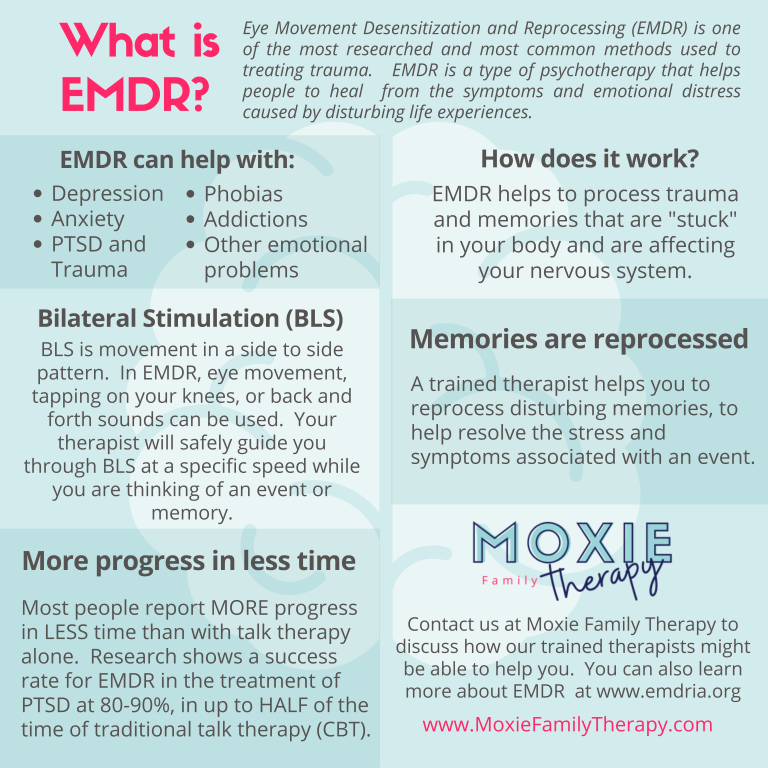
Research supports the effectiveness of several evidence-based therapies for trauma-related disorders, including Eye Movement Desensitization and Reprocessing (EMDR) and prolonged exposure therapy (Bisson et al., 2007).
Evidence-Based Trauma Therapies
EMDR therapy helps your brain process traumatic memories without becoming overwhelmed by them. During EMDR sessions, you’ll recall traumatic experiences while engaging in bilateral stimulation (usually eye movements), which helps your brain integrate these memories more effectively.
The American Psychological Association recognizes EMDR as an effective treatment for PTSD, with many clients experiencing significant improvement in relatively few sessions.
Prolonged Exposure (PE) therapy gradually helps you confront trauma-related memories and situations you’ve been avoiding. This might sound scary, but it’s done in a carefully controlled, supportive environment with a trained professional.
Trauma-Focused CBT combines cognitive behavioral techniques with trauma-specific interventions, helping you process traumatic experiences while developing healthier thinking patterns and coping skills.
Finding the Right Therapist
Not all therapists specialize in trauma treatment, so it’s important to find someone specifically trained in evidence-based trauma therapies. Look for credentials like:
- Licensed Clinical Social Worker (LCSW) with trauma specialization
- Licensed Professional Counselor (LPC) certified in EMDR or other trauma therapies
- Psychologist with post-doctoral training in trauma treatment
Ask potential therapists directly about their trauma training and experience. A good trauma therapist will be happy to discuss their qualifications and approach.
Overcoming Barriers to Treatment
Cost concerns are real, but many communities offer sliding-scale therapy options. If you’re a veteran, you may qualify for VA mental health services. For more information about navigating the VA disability process guide, understanding your benefits can open doors to crucial mental health resources.
Time constraints feel overwhelming when you’re managing work, family, and daily survival. But consider this: investing 1-2 hours per week in therapy can give you back countless hours currently lost to trauma symptoms.
Cultural or religious concerns can be addressed by finding therapists who understand and respect your background. Many faith-based counselors integrate spiritual principles with evidence-based trauma treatment.
The Role of Faith and Spirituality in Trauma Recovery ✝️
As someone whose faith has been both tested and strengthened through difficult experiences, I believe spiritual resources can be powerful allies in trauma recovery. This isn’t about pushing religion on anyone—it’s about acknowledging that for many people, spiritual practices provide meaning, hope, and community during healing.
Prayer and meditation offer similar benefits to secular mindfulness practices, with the added dimension of connection to something greater than yourself. Research from ISRN Psychiatry shows that religious coping strategies can significantly reduce PTSD symptoms.
Faith communities provide natural support networks, though it’s important to find congregations that understand trauma rather than offering simplistic “just pray about it” responses.
Spiritual practices like journaling, gratitude exercises, and service to others can complement professional therapy and other emotional healing strategies.
Creating Your Personal Trauma Recovery Plan 📋
Trauma recovery isn’t one-size-fits-all. What worked for me as a male veteran might look different from what works for you. The key is creating a personalized plan that addresses your specific needs, circumstances, and goals.
Assessment: Where Are You Now?
Honestly evaluate your current symptoms and functioning:
- How is trauma affecting your daily life?
- What triggers tend to activate your trauma responses?
- Which areas of your life (work, relationships, parenting, health) need the most attention?
- What resources and support systems do you currently have available?
Goal Setting: Where Do You Want to Be?
Set realistic, specific goals for your healing journey:
- Short-term goals (1-3 months): Maybe it’s sleeping through the night or having one social interaction per week
- Medium-term goals (3-12 months): Perhaps returning to activities you once enjoyed or improving a key relationship
- Long-term goals (1+ years): Could include career changes, major life decisions, or helping others with similar experiences
Strategy Integration: How Will You Get There?
Combine multiple approaches for maximum effectiveness:
- Professional therapy as your foundation
- Social support as your safety net
- Physical exercise as your energy source
- Mindfulness practices as your daily tool
- Cognitive techniques as your mental framework
Monitoring Progress: How Will You Know It’s Working?
Track your healing journey through:
- Symptom journals noting frequency and intensity of trauma responses
- Mood tracking to identify patterns and triggers
- Relationship quality improvements in your connections with others
- Functional improvements in work, parenting, or daily activities
Building Resilience for Long-Term Recovery 🛡️
Trauma recovery isn’t just about returning to your pre-trauma state—it’s about building resilience that makes you stronger than before. This concept, called post-traumatic growth, recognizes that surviving trauma can actually enhance your capacity for joy, connection, and purpose.
The Five Areas of Post-Traumatic Growth
Appreciation of life often deepens after trauma. Many survivors report greater gratitude for simple pleasures and everyday moments. This isn’t toxic positivity—it’s a genuine shift in perspective that comes from understanding life’s fragility and preciousness.
Relating to others can become more authentic and meaningful. Trauma strips away pretense and helps you value genuine connection over surface-level relationships.
Personal strength awareness develops as you realize you survived something you never thought you could handle. This knowledge becomes a source of confidence for future challenges.
New possibilities often emerge from trauma experiences. Many survivors discover new careers, passions, or life directions they never would have considered otherwise.
Spiritual development frequently accompanies trauma recovery, whether through traditional religion or broader spiritual practices. This doesn’t require specific beliefs—just openness to questions of meaning and purpose.
Maintaining Progress
Trauma recovery requires ongoing attention, even after initial healing. Think of it like physical fitness—you don’t stop exercising once you get in shape.
Regular check-ins with yourself help you notice when stress or triggers are affecting your well-being. Monthly or quarterly self-assessments can prevent small setbacks from becoming major relapses.
Continued support remains important even after formal therapy ends. Maintain connections with supportive people and consider periodic “booster sessions” with your therapist.
Stress management becomes a lifelong skill. Continue practicing the coping strategies that worked during your active recovery phase.

Supporting Others in Their Trauma Recovery Journey 🤗
If someone you love is struggling with trauma, your support can make a tremendous difference in their healing process. But supporting a trauma survivor requires specific knowledge and skills.
What Helps
Listen without trying to fix. Sometimes the most healing thing you can offer is witnessing someone’s pain without immediately trying to make it better.
Respect their pace. Trauma recovery happens on the survivor’s timeline, not yours. Pushing for faster progress often backfires.
Educate yourself. Learn about trauma’s effects on the brain and behavior. This knowledge helps you respond with compassion rather than frustration when trauma symptoms appear.
Maintain boundaries. Supporting a trauma survivor can be emotionally draining. Take care of your own mental health so you can be consistently available.
What Hurts
Minimizing their experience with statements like “it could have been worse” or “you should be over this by now” damages trust and delays healing.
Taking their symptoms personally. When trauma survivors withdraw or become irritable, it’s usually about their internal struggle, not about you.
Enabling avoidance. While you want to protect your loved one from pain, completely shielding them from recovery challenges prevents growth.
For practical ways to offer support, consider exploring uplifting words that change your day—sometimes simple encouragement makes all the difference.
Special Considerations for Different Populations 🎯
Trauma recovery looks different across various demographics and life circumstances. Understanding these differences helps ensure everyone receives appropriate, effective care.

Veterans and Military Families
Military trauma often involves moral injury—damage to your sense of right and wrong based on witnessing or participating in events that violated your values. This requires specialized treatment approaches that address both PTSD symptoms and moral distress.
Military Sexual Trauma (MST) affects both male and female service members and requires culturally competent therapists who understand military culture and dynamics.
Family impact extends trauma beyond the individual veteran. Spouses and children of trauma survivors often develop secondary trauma symptoms that need attention.
Childhood Trauma Survivors
Complex PTSD often develops from prolonged childhood trauma and requires longer-term treatment approaches that address developmental impacts, not just specific traumatic events.
Attachment issues frequently accompany childhood trauma, affecting adult relationships and parenting abilities. Specialized therapies like Dialectical Behavior Therapy (DBT) can be particularly helpful.
Cultural and Ethnic Considerations
Historical trauma affects entire communities and can influence individual healing journeys. Understanding cultural context helps therapists provide more effective, respectful treatment.
Language barriers can complicate therapy, making it important to find bilingual therapists or qualified interpreters who understand mental health terminology.
Cultural stigma around mental health varies significantly across communities. Healing approaches must respect cultural values while still providing effective treatment.
The Economics of Trauma Recovery 💰
Let’s be honest about the financial realities of trauma treatment. Quality therapy costs money, and many insurance plans provide inadequate mental health coverage. But consider the cost of NOT addressing trauma:
Lost productivity from trauma symptoms can affect career advancement and earning potential over decades.
Physical health problems often develop from untreated trauma, leading to expensive medical bills and chronic conditions.
Relationship costs include potential divorce, family conflict, and social isolation that affect quality of life and practical support.
Substance abuse frequently accompanies untreated trauma, creating additional financial and health burdens.
Finding Affordable Treatment Options
Community mental health centers often provide sliding-scale therapy based on income and family size.
Training clinics at universities offer quality therapy from supervised graduate students at reduced costs.
Employee Assistance Programs (EAPs) through many workplaces provide free short-term counseling.
Veteran benefits include comprehensive mental health services for qualifying veterans and sometimes their families.
Religious organizations sometimes offer faith-based counseling, though ensure counselors have proper training in trauma treatment.
Technology and Trauma Recovery 📱
Modern technology offers new tools for trauma recovery, though they should supplement, not replace, professional treatment and human connection.
Helpful Apps and Online Resources
Meditation apps like Headspace, Calm, or Insight Timer provide guided mindfulness practices specifically designed for trauma survivors.
PTSD Coach is a free app developed by the VA that helps track symptoms, provide coping tools, and connect users with resources.
Telehealth therapy makes professional treatment more accessible, especially for those in rural areas or with transportation challenges.
Online support groups connect trauma survivors across geographical boundaries, though be cautious about unmoderated forums that might not provide healthy support.
Technology Precautions
Social media can trigger trauma responses through unexpected content or negative interactions. Consider limiting exposure during active recovery phases.
News consumption should be moderated, as constant exposure to traumatic news stories can retraumatize survivors and increase anxiety.
Gaming or streaming can become unhealthy escape mechanisms if used to avoid processing emotions or engaging in recovery work.
Creating Trauma-Informed Families and Communities 🏡
Trauma recovery happens best within supportive environments that understand and accommodate trauma’s effects. As parents, partners, and community members, we can create spaces that promote healing.
Trauma-Informed Parenting
Emotional safety becomes the top priority. Children need to know they can express difficult emotions without judgment or punishment.
Predictable routines help traumatized family members feel secure and in control. This doesn’t mean rigidity—it means reliable patterns that provide stability.
Open communication about mental health normalizes seeking help and reduces stigma. Age-appropriate discussions about trauma and recovery help children understand and cope.
Building Supportive Communities
Education and awareness help community members recognize trauma symptoms and respond helpfully rather than judgmentally.
Resource development includes advocating for better mental health services, trauma-informed schools, and workplace mental health programs.
Reducing stigma happens through sharing stories, supporting legislation that improves mental health care, and challenging harmful stereotypes about trauma survivors.
Moving Forward: Your Next Steps 🚀
Reading about trauma recovery strategies is just the beginning. Real healing requires action, courage, and commitment to your own well-being.
Immediate Actions You Can Take Today
- Reach out to one supportive person and let them know you’re working on healing
- Practice one mindfulness technique for just 5 minutes
- Take a short walk or do light physical movement
- Write down three things you’re grateful for, no matter how small
- Research therapists in your area who specialize in trauma treatment
This Week’s Goals
- Schedule a consultation with a trauma-informed therapist
- Identify your support network and reach out to key people
- Start a basic exercise routine, even if it’s just 10 minutes daily
- Begin practicing one relaxation technique consistently
- Set boundaries around activities or people that feel traumatic

Long-Term Commitment to Healing
Trauma recovery isn’t a destination—it’s a journey that requires ongoing attention and care. Some days will be harder than others, and that’s completely normal. What matters is your willingness to keep moving forward, to keep choosing healing over survival mode.
Remember that seeking help is a sign of strength, not weakness. It takes tremendous courage to face trauma and work toward healing. You’ve already survived the worst—now it’s time to learn how to thrive.
Final Thoughts: You Are Not Alone 🙏
As I wrap up this comprehensive guide to trauma recovery, I want you to know something important: your trauma doesn’t define you, but your healing can transform you.
The five evidence-based strategies we’ve covered—building support networks, practicing mindfulness, engaging in physical exercise, using cognitive behavioral techniques, and seeking professional help—provide a roadmap for healing. But remember, everyone’s journey looks different.
Some of you reading this are just beginning to acknowledge that trauma has affected your life. Others have been in recovery for years but need new tools or encouragement. Wherever you are in this process, you deserve compassion, support, and hope.
God bless you on this journey. Healing is possible, help is available, and you are worthy of peace, joy, and authentic connection with others.
Your trauma may have changed your story, but it doesn’t get to write your ending. That’s up to you.
If you’re in crisis, please reach out immediately:
- National Suicide Prevention Lifeline: 988
- Crisis Text Line: Text HOME to 741741
- National Sexual Assault Hotline: 1-800-656-HOPE (4673)
- Veterans Crisis Line: 1-800-273-8255
Remember: Each person’s experience with trauma is unique, so it’s essential to consult with a qualified mental health professional to determine the most appropriate approach for addressing your specific emotional trauma.
More from the Blog:
- Family Routines That Work – 7 Simple Fixes for a Calmer Day
- Unlocking VA Disability Process: 5 Proven Tips for Success
- Responsible Pet Ownership: 10 Truths Every Family Should Know🐶 🐱 🦜
🌐 Explore More from Our Family of Blogs
If you found this article helpful, you might also enjoy what we’re sharing across our other platforms. Each one is designed to uplift, equip, and inspire families in real, practical ways:
🏠 Mountains Will Move
Faith-based encouragement for everyday families. We dive into prayer, parenting, purpose, and pressing through life’s hardest seasons with Jesus at the center.
👉 Visit Mountains Will Move »
🔎 Everyday Exposed
Our no-filter truth hub—where we tackle myths, challenge misleading narratives, and bring clarity to the conversations that matter most.
👉 Visit Everyday Exposed »
Whether you’re diving deeper into pet care, faith, or uncovering truth in today’s noisy world, I hope you’ll journey with us.
Thank you for being part of the community. God Bless you and your family. 🙏

